There's widespread misunderstanding of the energy balance model (EBM) of obesity. The EBM does NOT postulate that food intake is primarily under conscious control or that obesity is a failure of willpower and can be effectively treated by calorie counting or advice to “eat less”.
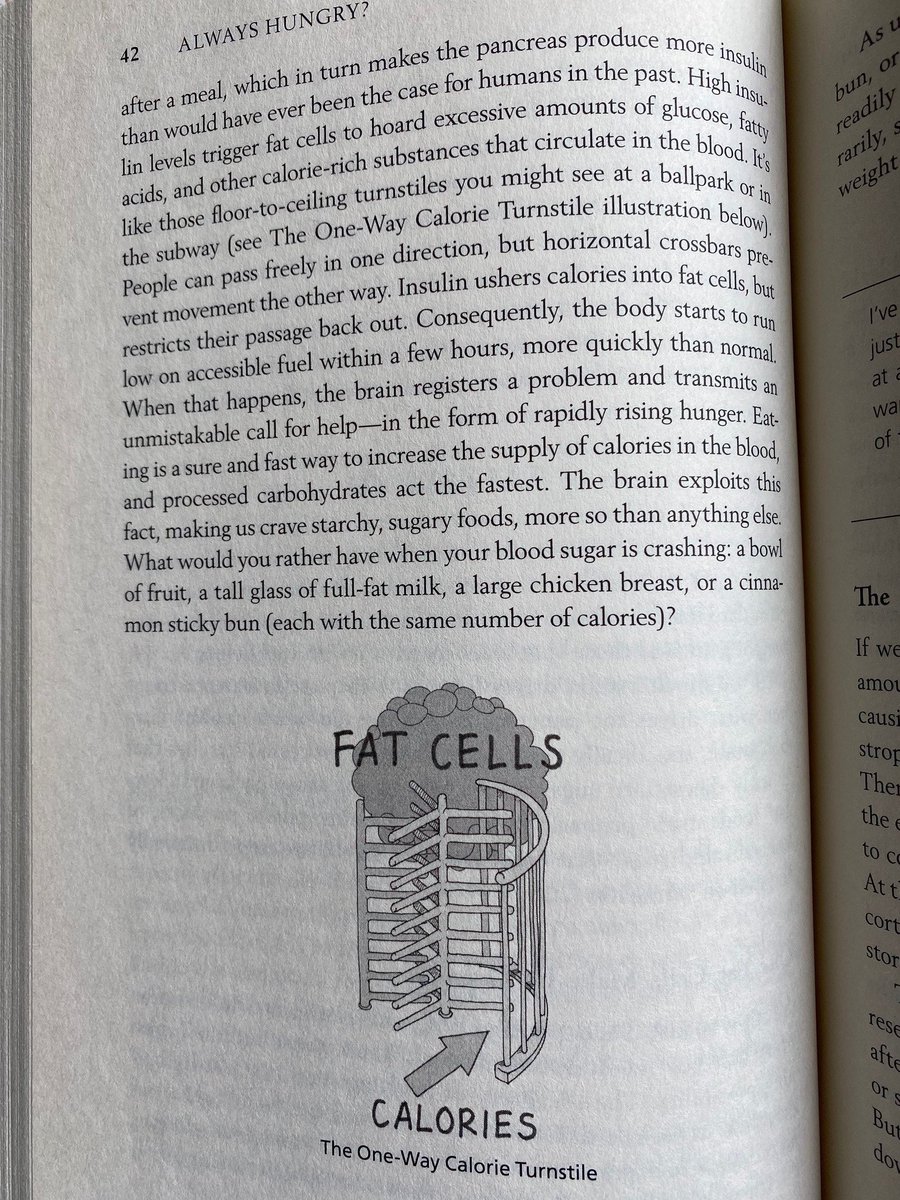
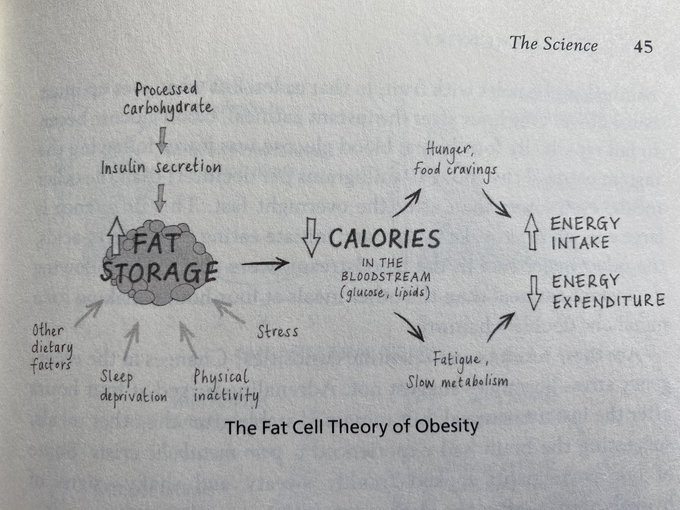
The EBM postulates that the food environment & the foods we eat affect feedback control of appetite & body weight regulation mediated by a variety of hormones & other signals acting on brain regions involved in sensory processing, reward, incentive salience, habit & homeostasis.
The EBM does NOT imply that all calories are equal. Different foods and nutrients can differentially affect the neural systems responsible for controlling food intake as well as affect metabolic health independent of body weight.
Alas, the EBM is far from complete because we are only beginning to understand the neural systems responsible for appetite control & the mechanisms underlying the influence of internal signals and their interaction with nutrients and the food environment.
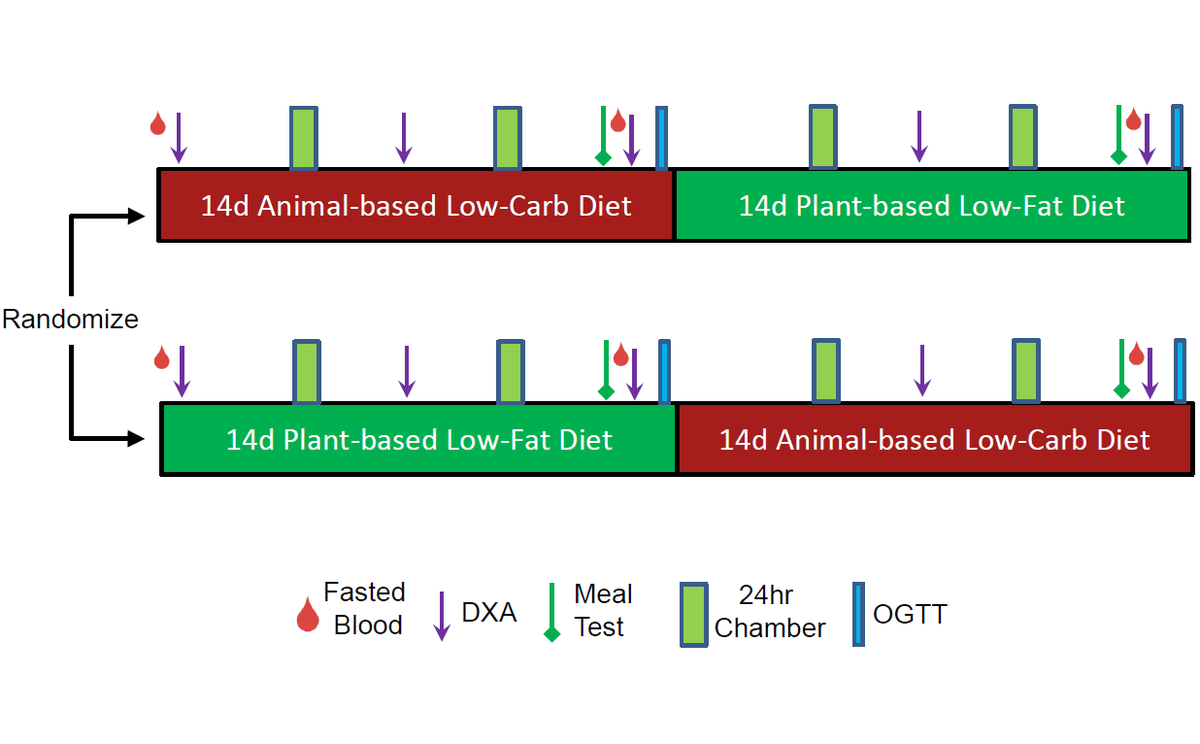
A sketch of the EBM was described in the @ScienceMagazine paper I wrote with @JohnSpeakman4 showing how hormones (like insulin) play a role in obesity while circumventing the problems with the carbohydrate-insulin model. science.sciencemag.org/content/372/65… 

• • •
Missing some Tweet in this thread? You can try to
force a refresh