
Thromboembolic disease has defined the last year for our practice. #COVID has given us the time and unfortunately the patients to refine our interventional strategies. I get asked from time to time to describe the steps involved in a basic #PE case. So here goes....(thread)
(I'll cover concepts in patient selection another time). This illustrative case is a mid 50-s male with acute onset dyspnea 3 weeks after testing positive for #COVID19. No syncope, no pertinent medical history. OSa in the low 80s on RA. HR 115. RV:LV Ratio ~1.5 #iRad (1/ ) 

CTA shows bilateral, predominantly lobar distribution PE. Probably a small evolving infarct in the left lower lobe. (2/ )
As for catheter selection, T24Flex is my go-to choice, with only a few uncommon exceptions. I've found T24 cases are quicker, with larger vol clot extraction, Flex tracks super well, and still allows coaxial T20 Curve access for stubborn LLL disease #iRad #cardiotwitter (3/ )
I start the case with US-guided right CFV access, place a micro puncture and take an liliocavagram. Why? Habit I guess... also think that it's probably wise to check a vessel every time before you advance something 20-24Fr. Next I start small with a 6Fr 10cm sheath. (4/ )
From there I advance the angled pigtail into the main PA and measure pressure. In this case was 64/33 mmHg. I do a PA-gram but its a hand injection and only to confirm where I am before measuring. I use CTA info and try to approach the thrombectomy similarly for all cases (5/ )
Next, I take the angled pig into the RLL PA (Cordis 6Fr 110cm). I take another hand injection to confirm location of my catheter. I then *important* remove the catheter over the 1cm floppy, exchange-length amplatz taking care to maintain the distal wire knuckle (6/ ) 
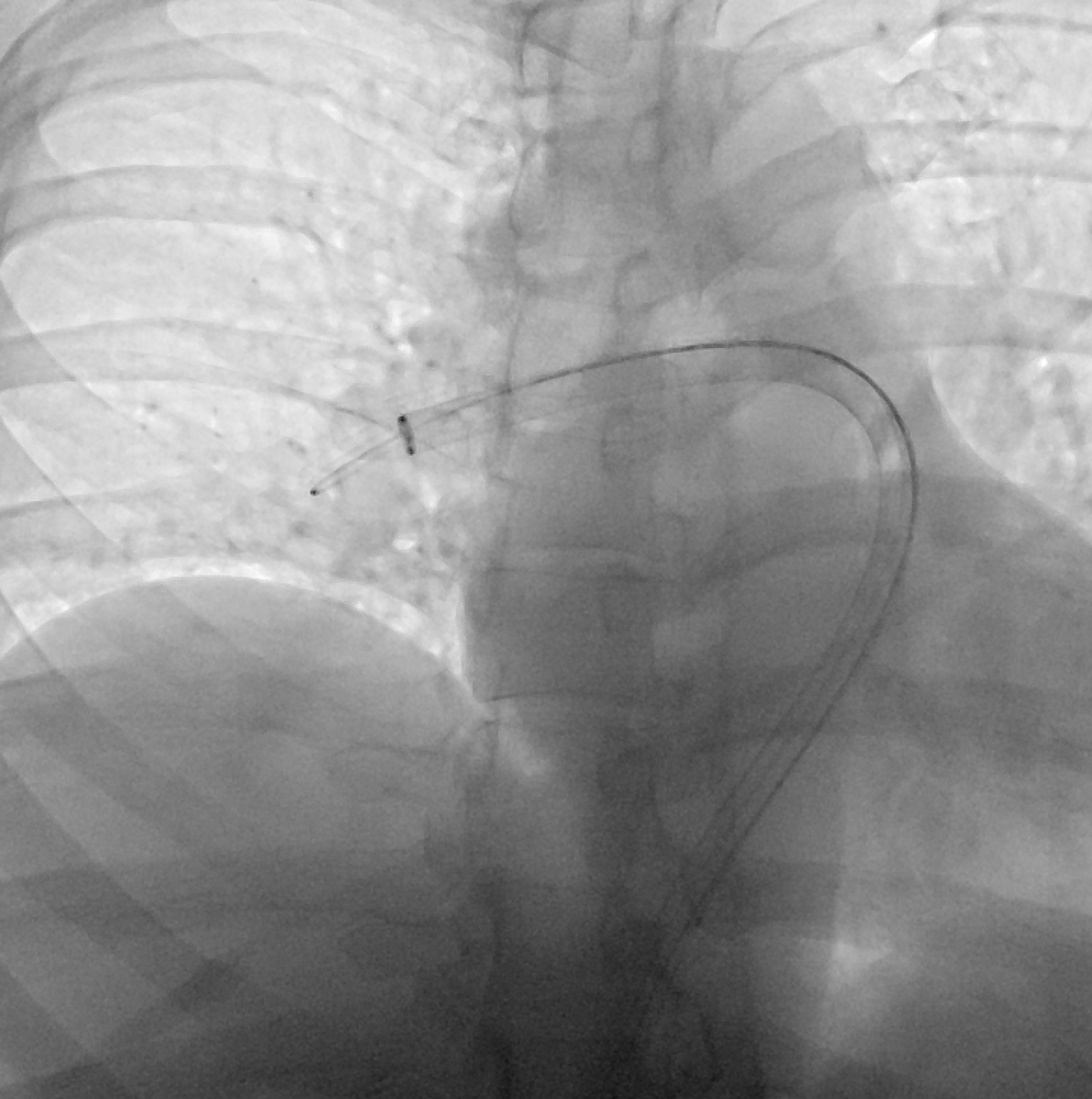
The wire knuckle is key, as it allows you to place a little forward tension on your thrombectomy catheter as you advance it from main PA to the RLL PA. Now, I remove the 6Fr sheath, place the 24 Fr Dryseal and advance my T24 flex into the RLL pulmonary artery. (7/ )
I make at least two aspirations in the RLL, more if needed to remove the expected volume of clot I see on CTA. Then slowly retract under fluoro until you see/feel engagement of the truncus anterior (8/ )
From there, I take a right PA-gram through the T24 by loading ~15cc of contrast into the catheter and flushing it under DSA (6frames/sec) with a 20cc syringe of saline. This lets me check my work in the RLL and visualize clot in the RUL (9/ )
Angiogram show a large volume of RUL clot. Here ill often retract the wire from the RLL and CAREFULLY advance into the truncus. The angles help from from RLL to RUL. Then put a little forward tension on the T24 to engage the truncus and aspirate 1-2 times (10/ )
I should stress that this is a move that requires a little finesse, and should be done carefully and only after the operator has done enough cases to have a feel for how the catheter reacts, so as to avoid an inadvertent wire or catheter injury (11/ )
Once the clot has been removed from the RUL, I like to confirm with a hand injection through the T24, using ~10cc contrast (again flushed by 20cc saline). This confirms restoration of flow without signiificant residual thrombus (12/ )
Next, I return the white obturator to the T24, which nearly always straightens the catheter out and causes it to retract into the main PA. I've found that 60-70% of the time the wire will advance directly from there to the LLL. I watch it by putting a little LAO on the II (13/ )
I carefully advance the T24 into the LLL, paying attention to the way the catheter feels, stopping with any resistance. Here I use the bronchial tree as a rough landmark. I remove the obturator and aspirate. Pull back a little and aspirate. Pull back into LUL and aspirate (14/ )
Next, retract into the main left PA and take an angiogram (15cc contrast, flushed with 20cc saline). This is a big decision fork: If it looks great, then I measure pressure and finish. If it looks bad I repeat and make another pass or 2. If I'm not sure I measure pressure (15/ )
LPA-gram much improved from CTA. Still a little clot distally in the LLL, but large vol clot removed and on the table. Here I measured pressure to help decide whether to take the curve or T16 into the distal LLL. Mean Pa pressure dropped 16mmHg. Hemodynamics normalized (16/ )
>10mmHg drop in mean PAP, normalization of hemodynamics, large vol clot out --> I ended the procedure. Thrombectomy is about being careful, not fast - BUT some patients will decline w prolonged catheter dwell time, so getting comfortable w a resonable end point is key (17/ )
After measuring pressure, I removed the sheath and used a FlowStasis device to seal. Total procedure time here was 26 mins. Catheter dwell time was 18 mins and fluoro time <10mins. Not the fastest time, nor is that ever the goal. Patient did well & discharged 36hrs later (18/ ) 

I hope this overview is maybe kinda helpful - Its the synthesis of our experience over the past couple years (when these cases all lasted >1hr😬). Not every case goes perfect, and there are roles for the other devices that I'd be happy to discuss separately! (end)
Main things I’ve found helpful: 1) Relying on CTA rather than a lot of angiograms to minimize contrast load 2) Approach in a standardized way - RLL-> RUL -> LLL -> LUL. 3) know when to finish
• • •
Missing some Tweet in this thread? You can try to
force a refresh



