This 👇claim arises principally from Israeli data (which is unpublished in any form so will withhold judgment) and from the UK REACT 1 study, rounds 12 & 13. But... is the REACT 1 data likely to be solely explained by delta? 🧵
(study link spiral.imperial.ac.uk/handle/10044/1…)
(study link spiral.imperial.ac.uk/handle/10044/1…)
https://twitter.com/EricTopol/status/1425492860619481098
This is the table in question. You can see VE of a combination of AZ/MRNA vs symptomatic infection was 83% (19-97%) in round 12, but only 59% (23-78%) in round 13. The concern of course is that this drop in VE is due to delta, which had completely taken over by round 13 /2 
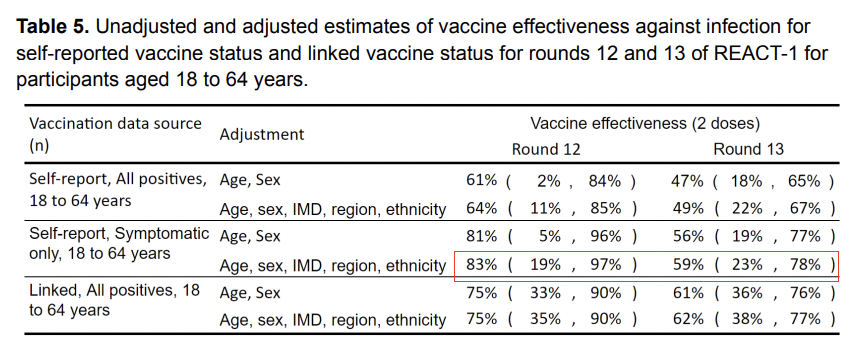
However, while 100% of the isolates identified in round 13 were delta, 80% in round 12 were also delta (20% were alpha). Any effect of delta on VE should have been partially seen in round 12. /3
So, if the overall VE of these mixed vaccines vs delta was actually 60% (and 90% vs alpha) as suggested in original QT, we would expect a point estimate in round 12 closer to 0.5*0.8+0.9*0.2=0.58. Instead, while 0.58 is within the 95% CI, we see a point estimate of 0.83. /4
As a result, its unlikely likely that the drop in VE b/w rounds 12 & 13 is solely explained by delta itself. This is supported by the best available data on the ?, which found a small drop in VE vs symptomatic infx w delta in a test-negative design /5
https://twitter.com/AaronRichterman/status/1417967455322968065?s=20
So what are some possible explanations for the drop in VE between rounds 12 and 13?
1. natural immunity among unvaccinated
1. natural immunity among unvaccinated
https://twitter.com/ct_bergstrom/status/1422978581253087236?s=12/6
2. wide confidence intervals, so perhaps we are just seeing imprecise estimates
3. immunity waning after vaccination for (elderly) folks who got vaccinated towards beginning of 2021
4. indirect protection from population immunity biasing VE estimate
3. immunity waning after vaccination for (elderly) folks who got vaccinated towards beginning of 2021
4. indirect protection from population immunity biasing VE estimate
https://twitter.com/AaronRichterman/status/1423060643406438404?s=20/7
• • •
Missing some Tweet in this thread? You can try to
force a refresh