"The @PCORI Board’s approval of $61.3 million will enable eight PCORnet CRNs to optimize their infrastructure resources and capacities to support PCORnet in its third phase." What is the total spent on PCORnet to date? What are the deliverables to date? pcori.org/news-release/p… 
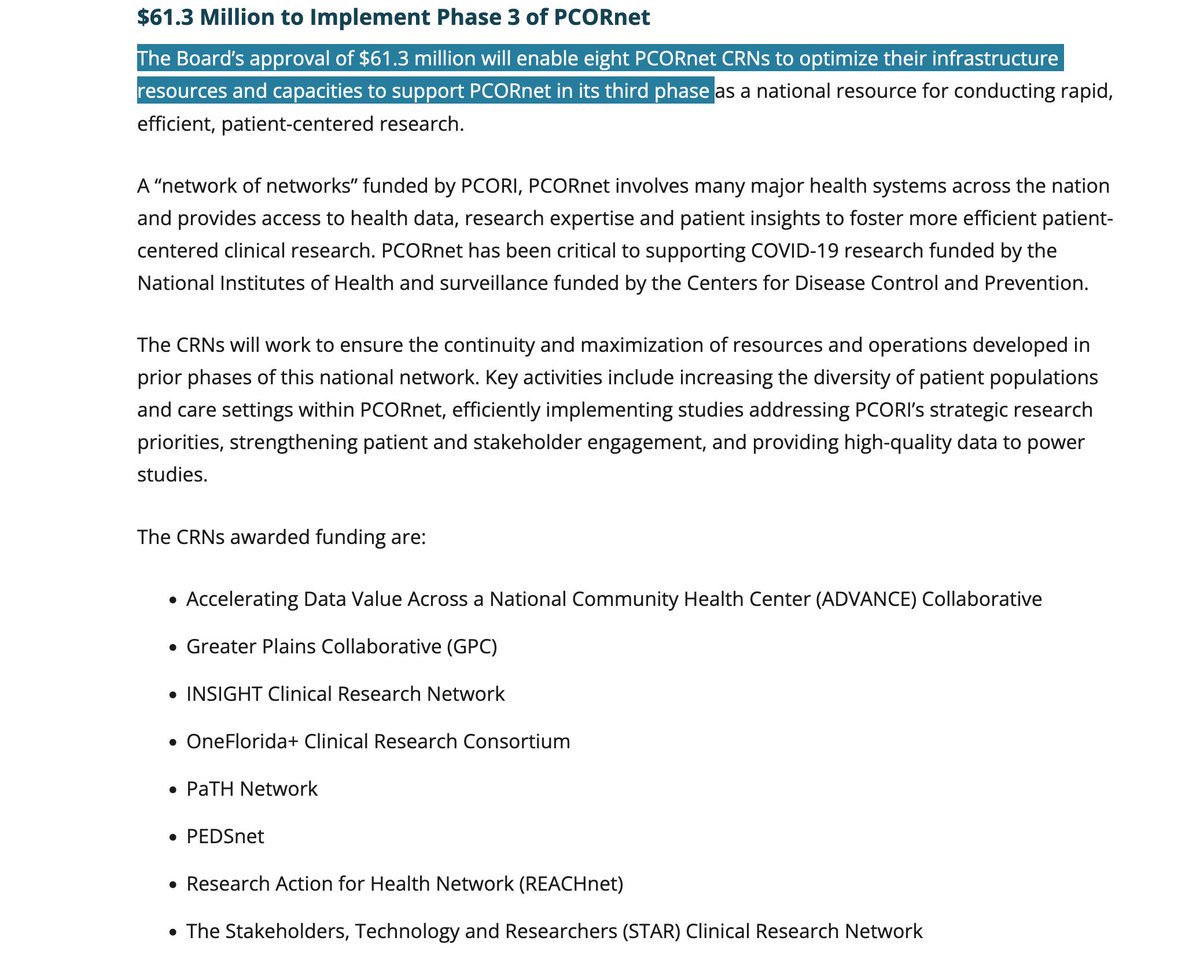
@PCORI And asking w/respect, just think the accounting of resources spent & deliverables provided is good hygiene for funders. And what resources from the effort are publicly available for others to leverage? Since this is such a big investment, regular reports on ROI is useful. @PCORI
@PCORI And this might be available, I just didn’t know where to look. By the way, similarly with @NIH, who previously reported that almost half of their funded trials were never published. Quarterly reports on trial funding and deliverables (results reported), for example, also great.
@PCORI @NIH And this is also helpful to others trying to create data networks; what is being spent, where did the money go, what did it produce, and for whom and in what timeframe. Transparency is ideal for lifting everyone as we iterate and improve going forward.
• • •
Missing some Tweet in this thread? You can try to
force a refresh