Our paper dropped: Performance Metrics for Comparative Analysis of Clinical Risk Prediction Models Employing Machine Learning. We show 'commonly reported metrics may not have sufficient sensitivity to identify improvement of
#ML models…’ @CircOutcomes ahajournals.org/doi/abs/10.116…
#ML models…’ @CircOutcomes ahajournals.org/doi/abs/10.116…
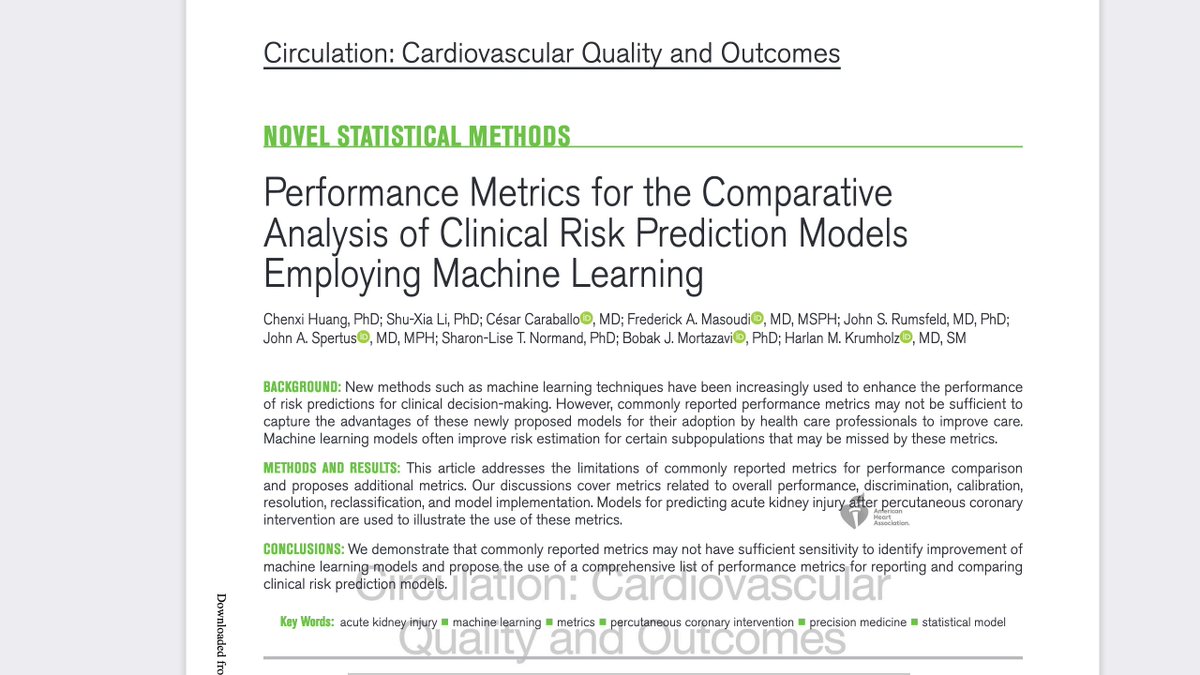
@CircOutcomes Risk models are ubiquitous now. In this paper, we 'propose the use of a comprehensive list of performance metrics for reporting and comparing clinical risk prediction models.’ Time to expand the metrics. @CircOutcomes ahajournals.org/doi/abs/10.116… @YaleMed @YaleCardiology @AHAScience 

@CircOutcomes @YaleMed @YaleCardiology @AHAScience We review a wide range of options for assessing the performance of risk models and demonstrate the neccessity of a comprehensive view in any evaluation. Paper was led by Chenxi Huang. Also with @jbmortazavi; SL Normand; @jspertus @CesarCaraballoC @Dr_BowTie65 @DrJRums 
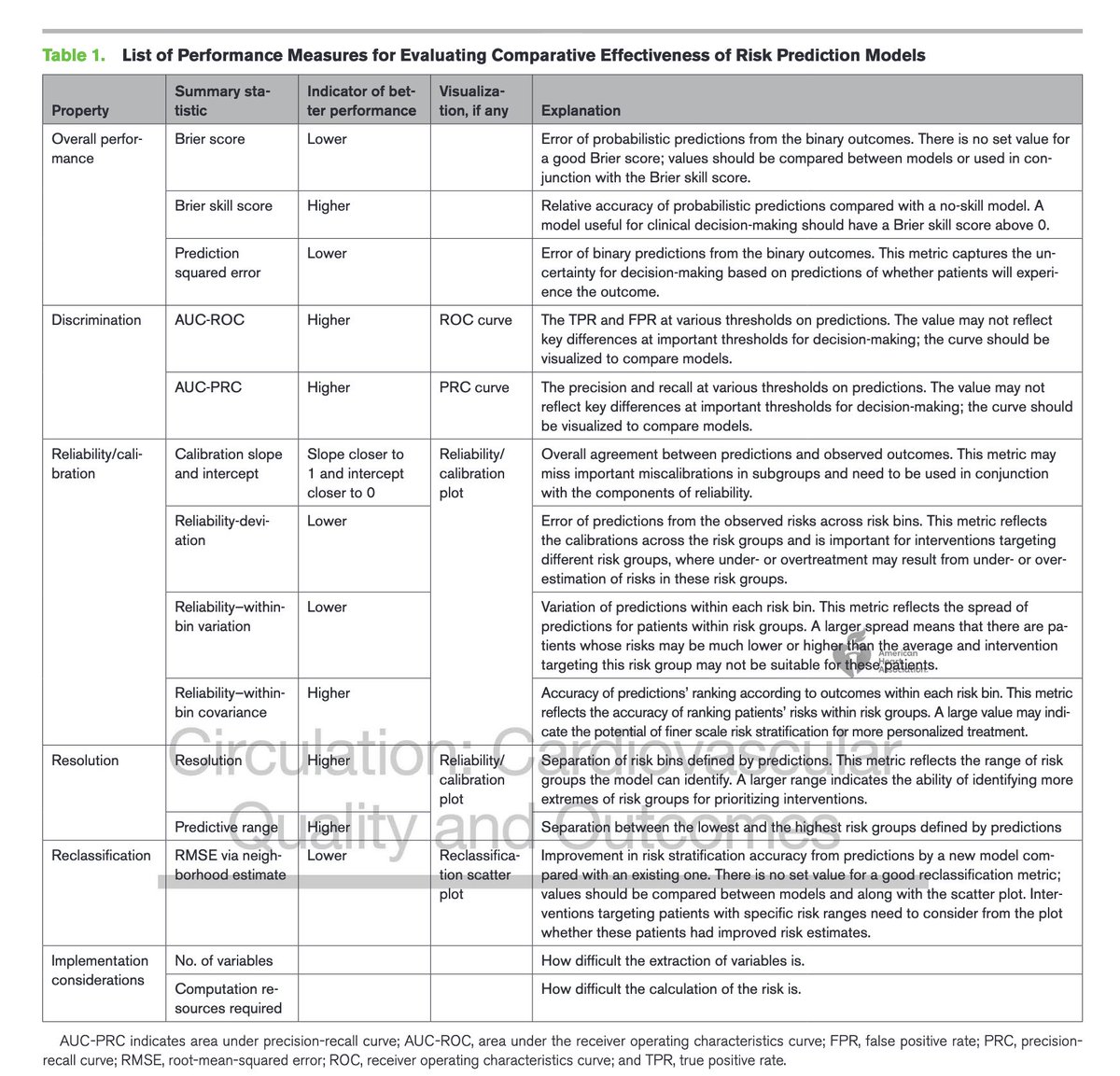
@CircOutcomes @YaleMed @YaleCardiology @AHAScience @jbmortazavi @jspertus @CesarCaraballoC @Dr_BowTie65 @DrJRums "Such a suite of metrics provides a comprehensive evaluation and comparison of the [risk] models, which is a critical step toward understanding the performance of a model when
implemented in practice.” @CircOutcomes
implemented in practice.” @CircOutcomes
@CircOutcomes @YaleMed @YaleCardiology @AHAScience @jbmortazavi @jspertus @CesarCaraballoC @Dr_BowTie65 @DrJRums Finally kudos to @CircOutcomes team for their help in improving the manuscript. I am an advocate for #preprints, but I am also an advocate for thoughtful, constructive peer review. And this article is open to the public, which is great because it seeks to set standards. @bnallamo
@CircOutcomes A premise of our paper is... traditional metrics of risk models may miss some of the advantages of #ML #AI models that capture better the risk of some patients, esp at the extremes of risk. In a precision approach, getting it right on each person matters. @YaleMed @YaleCardiology
• • •
Missing some Tweet in this thread? You can try to
force a refresh