
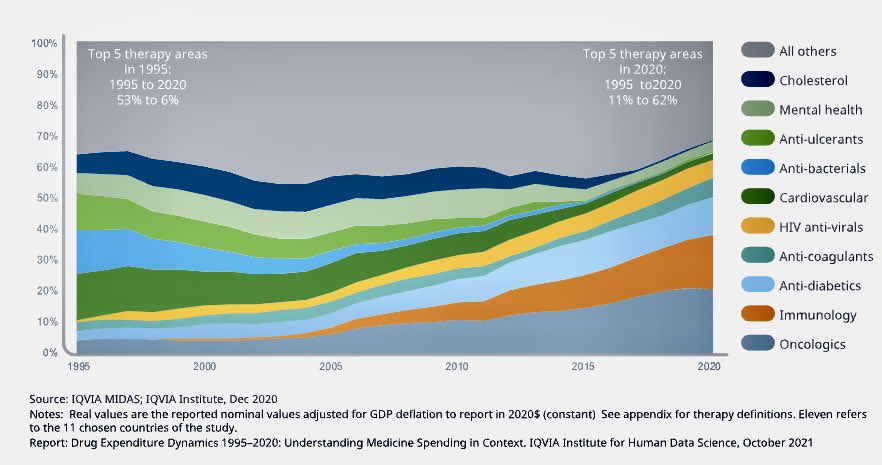
IQVIA report: Good news is drug spending as % of healthcare spending is stable at ~15%.
Worrisome: While $ spent on cholesterol, antibiotics, & ulcer meds is lower, the ones rising are ones that will continue go up: oncology, immunology, diabetes. iqvia.com/Insights/The-I…
Worrisome: While $ spent on cholesterol, antibiotics, & ulcer meds is lower, the ones rising are ones that will continue go up: oncology, immunology, diabetes. iqvia.com/Insights/The-I…

That's because cholesterol drugs and peptic ulcer drugs work chronically. Not just a few months and stop. So when you have a lot of generics, prices go down due to competition.
In contrast, oncology, immunology drugs are either ones that don't work for very long or are biologics
In contrast, oncology, immunology drugs are either ones that don't work for very long or are biologics
So there will continue to be newer and more expensive drugs each year and we are not seeing that effect yet. Every new cancer drug sold since 2017 has been >$100,000 per year. And that opening price has kept going up. These drugs also work only for a few months on average.
So there are newer and newer drugs. Which is good for patients. But unless there is value based pricing, paying >$100,000 for every drug including ones that are weak and hardly work is not sustainable. And is a barrier to true innovation because it lowers the risk.
And let's now go into diabetes. We have seen how insulin prices can be 10 times higher due to price increases. So the fact that spending on diabetes meds is going up is not unexpected. 
• • •
Missing some Tweet in this thread? You can try to
force a refresh









