Next up for me: Changing Landscape of Prone Positioning with @sqsimp @GallodeMoraesMD @md_ritwick and Dr. Bosch.
Follow this thread 🧵 for pearls from this session.
#CHEST2021 #CHESTtrainees
Follow this thread 🧵 for pearls from this session.
#CHEST2021 #CHESTtrainees

Abbreviations:
PP = Prone Positioning
APP = Awake Prone Positioning
ARDS = You know it!
ARF = Acute Resp Failre
So then, let's learn!
#CHEST2021
PP = Prone Positioning
APP = Awake Prone Positioning
ARDS = You know it!
ARF = Acute Resp Failre
So then, let's learn!
#CHEST2021
Dr. Bosch:
What is APP? Proning patients who are not mechanically ventilated (MV)
He's presenting a case, let me ask you in the meanwhile; Do you perform Awake Proning?
What is APP? Proning patients who are not mechanically ventilated (MV)
He's presenting a case, let me ask you in the meanwhile; Do you perform Awake Proning?
Bosch: Can APP help in patients who are not intubated and hypoxemic?
Benefits: ↑ oxygenation, avoiding MV, ?↓ mortality
Harm: P-SILI, delayed intubation, dislodged catheters/drains, pt discomfort
But what's the data for AWAKE PP?
#CHEST2021
Benefits: ↑ oxygenation, avoiding MV, ?↓ mortality
Harm: P-SILI, delayed intubation, dislodged catheters/drains, pt discomfort
But what's the data for AWAKE PP?
#CHEST2021
Elharrar (PMID: 32412581): Some respond in terms of oxygenation when awake prone, but question is does it affect patient outcomes.
PROSEVA did show in the past that improved oxygenation not related to mortality benefit, so equipoise remains.
#CHEST2021
PROSEVA did show in the past that improved oxygenation not related to mortality benefit, so equipoise remains.
#CHEST2021
Bosch discusses the recent trial: Ehrmann (PMID 34425070)
* S/F ratio moderate-severe ARDS
* 40% opts bese
* All pts on HFNC
* Median daily duration of awake proning: 5 hrs (1.6 - 8.6 hrs)
#CHEST2021
* S/F ratio moderate-severe ARDS
* 40% opts bese
* All pts on HFNC
* Median daily duration of awake proning: 5 hrs (1.6 - 8.6 hrs)
#CHEST2021

Ehrmann (PMID 34425070):
* Not diff in mortality but there was improvement in composite outcome
* Trend towards less treatment failure and intubations (pic 2)
* More benefit with longer period of APP (Pic 1)
* No increased AEs
#CHEST2021

* Not diff in mortality but there was improvement in composite outcome
* Trend towards less treatment failure and intubations (pic 2)
* More benefit with longer period of APP (Pic 1)
* No increased AEs
#CHEST2021


Do you do APP for people who are on nasal cannula?: Answer unclear.
2 studies available (PMID 33356977), Bosch's group has a study about to be published.
* Pts were able to be proned < 12 hours, pts actually weren't able to prone for > 2 hours
#CHEST2021
2 studies available (PMID 33356977), Bosch's group has a study about to be published.
* Pts were able to be proned < 12 hours, pts actually weren't able to prone for > 2 hours
#CHEST2021
Bosch:
So who should we awake prone?
* Early application probably better (some signals in studies,
Who is most likely to benefit?
* Lower P/F
* On HFNC vs. regular NC: More hypoxemia, likely more benefit
#CHEST2021
So who should we awake prone?
* Early application probably better (some signals in studies,
Who is most likely to benefit?
* Lower P/F
* On HFNC vs. regular NC: More hypoxemia, likely more benefit
#CHEST2021

Current trends in awake proning?
Prior to #COVID19: 44% ICU directors ready
Post #COVID19: 86% ICU directors ready to do APP
Summary slide on guidelines discussed at #CHEST2021
Prior to #COVID19: 44% ICU directors ready
Post #COVID19: 86% ICU directors ready to do APP
Summary slide on guidelines discussed at #CHEST2021

.@md_ritwick is up next at #CHEST2021: Physiologic basis of prone positioning (PP)
Clinically: Improve oxygenation
Other mechanisms:
* ↓ ventral dorsal TPP difference
* ↓ lung compression by heart/diaphragm
* ↑ pulmonary perfusion
#CHEST2021
Clinically: Improve oxygenation
Other mechanisms:
* ↓ ventral dorsal TPP difference
* ↓ lung compression by heart/diaphragm
* ↑ pulmonary perfusion
#CHEST2021

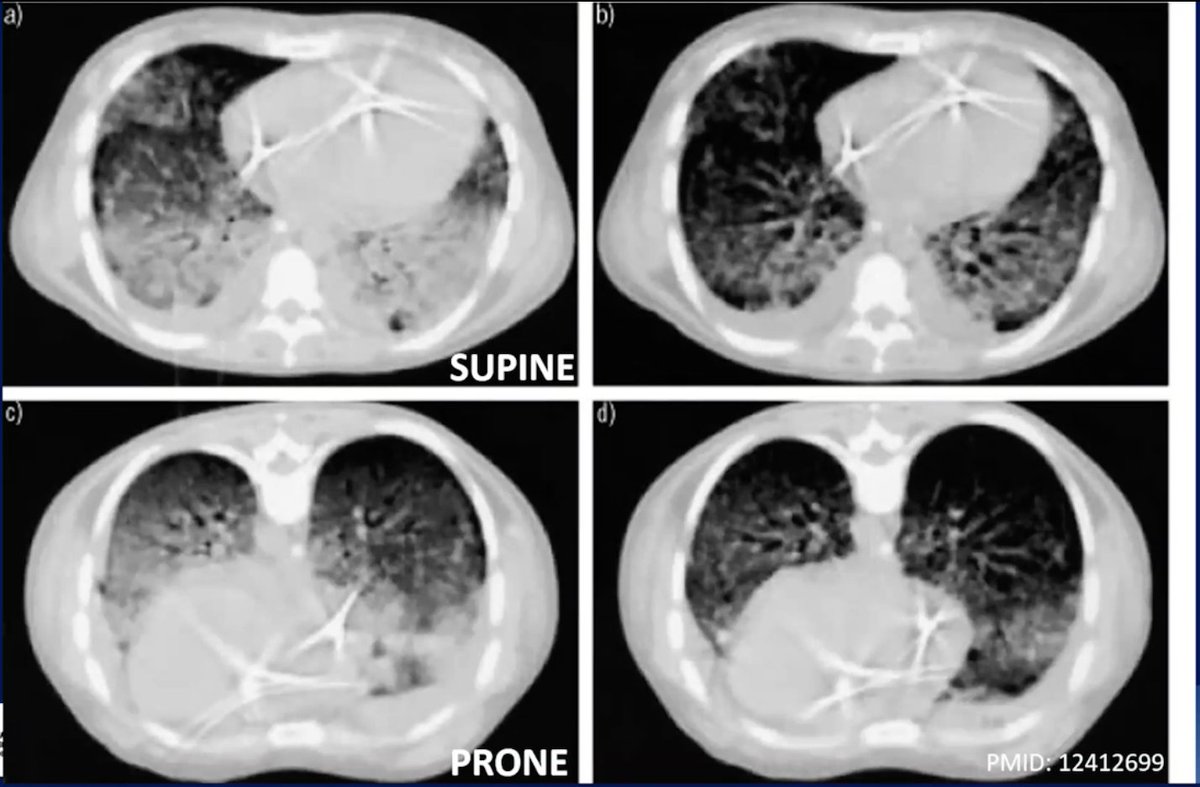
.@md_ritwick:
Mechanism 1: ↓ AP TPP gradient
* Pic 1 is demonstrative
* Pic 2: Schematic figure: ↓ TPP gradient in PP
Mech 2:
* ↓ lung collapse d/t heart/diaphragm --> ↓ shunt --> ↓ hypoxemia
#CHEST2021


Mechanism 1: ↓ AP TPP gradient
* Pic 1 is demonstrative
* Pic 2: Schematic figure: ↓ TPP gradient in PP
Mech 2:
* ↓ lung collapse d/t heart/diaphragm --> ↓ shunt --> ↓ hypoxemia
#CHEST2021

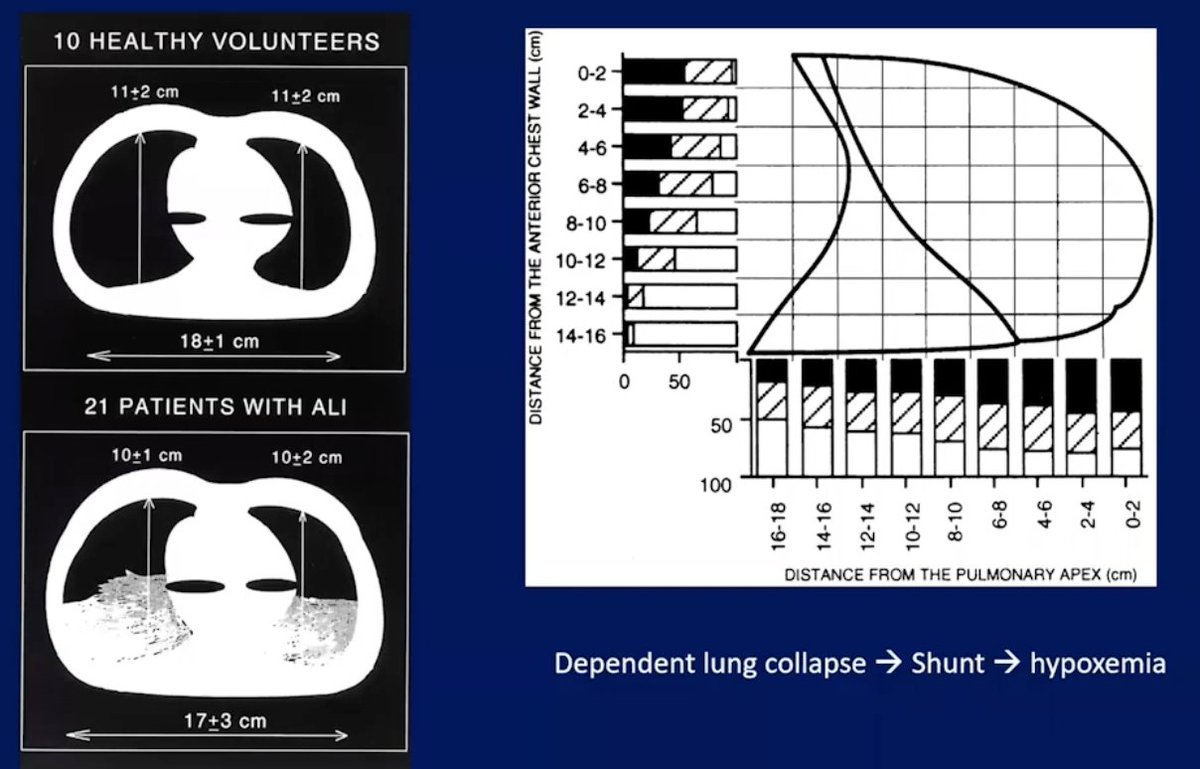
Do Mech 1 & 2 actually work? Yes, PMID: 8780285: Obese pts --> PP ↑ PFTs
Mech 3:
* ARDS:↑ perfusion in affected areas
* PP: Perfusion uniform across lung --> ↓ V/Q mismatch See figure.
Best learning reference (It's a classic): bit.ly/3vuRihE
#CHEST2021
Mech 3:
* ARDS:↑ perfusion in affected areas
* PP: Perfusion uniform across lung --> ↓ V/Q mismatch See figure.
Best learning reference (It's a classic): bit.ly/3vuRihE
#CHEST2021

Next up is my friend, mentor, and twin, @GallodeMoraesMD aka THE PRONING QUEEN! Might be the only one who pushes for proning more than I do!!!!
She's going to talk about PP in ARDS: When, how, when, and when to stop!
#CHEST2021
She's going to talk about PP in ARDS: When, how, when, and when to stop!
#CHEST2021
.@GallodeMoraesMD:
Benefit in PROSEVA (PMID: 23688302) likely attribute to the long durations of proning! So that's important to keep in mind
Prone group: ↓ 28d and 90d mortality and ↑ successful extubation + vent free days
#CHEST2021
Benefit in PROSEVA (PMID: 23688302) likely attribute to the long durations of proning! So that's important to keep in mind
Prone group: ↓ 28d and 90d mortality and ↑ successful extubation + vent free days
#CHEST2021
.@GallodeMoraesMD: HOW to prone:
* Don't need special beds, need a solid team
* "Burrito" the patient, bring pt towards the vent, members know which tube/line to keep track of, and then turn. It's a team dance!
* Pic 2: Use pillow w/ space to manage ETT
#CHEST2021

* Don't need special beds, need a solid team
* "Burrito" the patient, bring pt towards the vent, members know which tube/line to keep track of, and then turn. It's a team dance!
* Pic 2: Use pillow w/ space to manage ETT
#CHEST2021


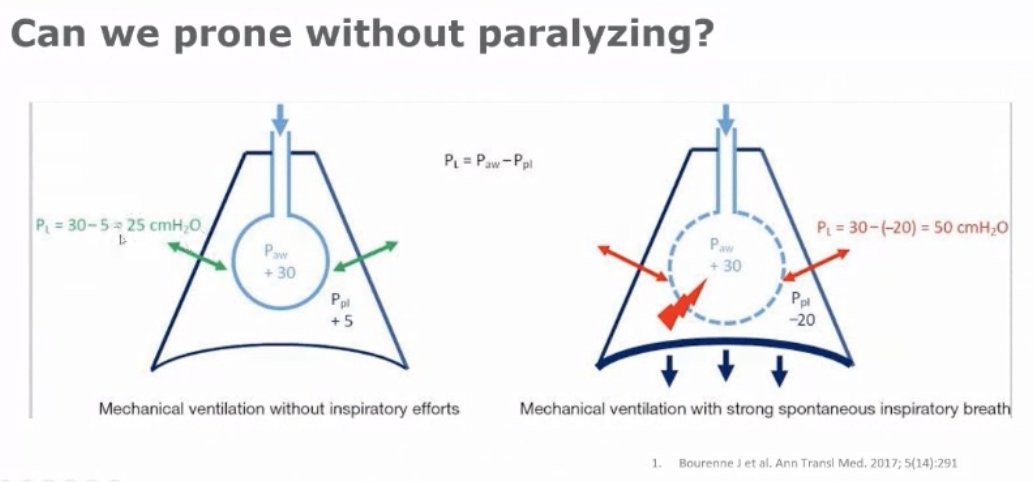
.@GallodeMoraesMD:
* We CAN prone without paralyzing BUT paralytics in hypoxemic failure can (Pic 2):
- ↑ ventilation in ARDS
- ↑ oxygenatn (don't need to use as drips as shown in ROSE): ? Mortality benefit
- ↑ V/Q match d/t ↓ work of breathing/TPP variations
#CHEST2021

* We CAN prone without paralyzing BUT paralytics in hypoxemic failure can (Pic 2):
- ↑ ventilation in ARDS
- ↑ oxygenatn (don't need to use as drips as shown in ROSE): ? Mortality benefit
- ↑ V/Q match d/t ↓ work of breathing/TPP variations
#CHEST2021

.@GallodeMoraesMD: Having a protocolized approach is key. Intubated someone for ARDS? Start considering proning per that protocol. She shares the protocol they implemented at @MayoPCCM .
Their group has published this protocol, find it here bit.ly/3C1BjtZ
#CHEST2021
Their group has published this protocol, find it here bit.ly/3C1BjtZ
#CHEST2021

.@GallodeMoraesMD: How long should you prone?
* As long as it is helping!: As long as P/F is benefiting
* Mortality benefit with P/F cutoff of 150, but that's not hard and fast
#CHEST2021
Dr. Gallo is closing out with these take-home points, and *mic drop*, Queen out!
* As long as it is helping!: As long as P/F is benefiting
* Mortality benefit with P/F cutoff of 150, but that's not hard and fast
#CHEST2021
Dr. Gallo is closing out with these take-home points, and *mic drop*, Queen out!

Here's a helpful infographic on proning from @accpchest ... There are a number of graphics that can be downloaded in high res at chestnet.org/topic-collecti…
#CHEST2021
#CHEST2021

• • •
Missing some Tweet in this thread? You can try to
force a refresh



















