1/ NEW: Excited to share our Viewpoint in @JAMA_current: "A Policy Prescription for Reducing Health Disparities -- Achieving Pharmacoequity."
A 🧵 on what #Pharmacoequity is, why it should be a public health & policy priority, and how we can achieve it.
jamanetwork.com/journals/jama/…
A 🧵 on what #Pharmacoequity is, why it should be a public health & policy priority, and how we can achieve it.
jamanetwork.com/journals/jama/…

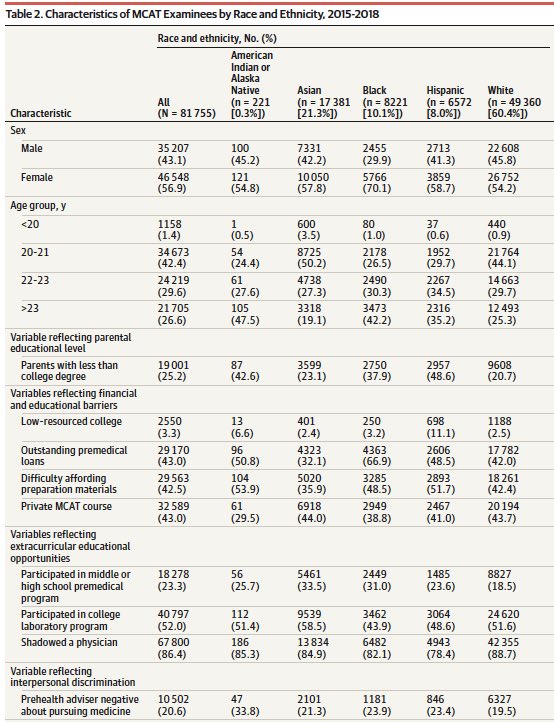
2/ Ensuring that all individuals, regardless of race & ethnicity, socioeconomic status, or availability of resources, have access to the highest quality medications required to manage their health needs is paramount. This is what we call #Pharmacoequity.
jamanetwork.com/journals/jama/…
jamanetwork.com/journals/jama/…

3/ The #COVID19 pandemic has brought health equity to the forefront, especially in how we ensure access to novel therapies, from antivirals like #remdesivir and #molnupiravir to the Covid vaccine...
But inequities in access to novel drugs are much more than a Covid problem. 👇🏾



But inequities in access to novel drugs are much more than a Covid problem. 👇🏾



4/ So how can we achieve #Pharmacoequity? We propose 3 key policy areas that we should focus on:
🔶 Increasing Access to drugs
🔶 Reducing Cost of drugs
🔶 Improving Quality of drugs
Here's what we mean.👇🏾
(Keep scrolling, you're halfway through! 😃)
jamanetwork.com/journals/jama/…
🔶 Increasing Access to drugs
🔶 Reducing Cost of drugs
🔶 Improving Quality of drugs
Here's what we mean.👇🏾
(Keep scrolling, you're halfway through! 😃)
jamanetwork.com/journals/jama/…

5/ First, we must reimagine "access." This includes:
1. Adopting universal, low-cost prescription drug coverage
2. ⬆️ geographical access to pharmacies
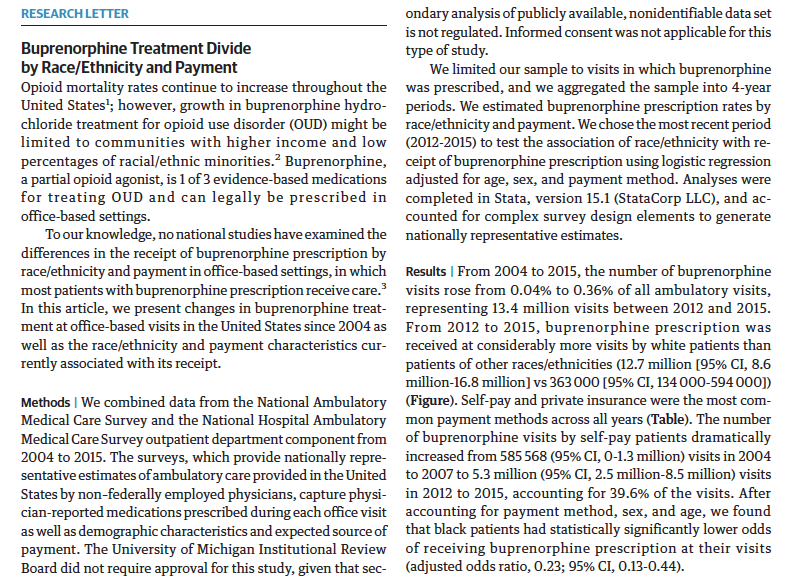
3. ⬇️ bias in specialist referral & novel drug prescribing
4. ⬆️ representation of underrepresented groups in clinical trials
1. Adopting universal, low-cost prescription drug coverage
2. ⬆️ geographical access to pharmacies
3. ⬇️ bias in specialist referral & novel drug prescribing
4. ⬆️ representation of underrepresented groups in clinical trials

6/ Second, we need a commitment to ⬇️ rising drug costs.
Many solutions to ⬇️ cost exist, but we believe that analyses of prescription drug prices & drug coverage policies need an *equity impact analysis* to examine the effect of all novel drugs on reducing health disparities.
Many solutions to ⬇️ cost exist, but we believe that analyses of prescription drug prices & drug coverage policies need an *equity impact analysis* to examine the effect of all novel drugs on reducing health disparities.

7/ Lastly quality improvement programs should prioritize #Pharmacoequity as a key part of QI measures.
We can do this by standardizing disparities data collection, intervening on known prescribing disparities, tracking & reporting equity improvements, and sharing best practices.
We can do this by standardizing disparities data collection, intervening on known prescribing disparities, tracking & reporting equity improvements, and sharing best practices.

8/ There's so much we didn't get to in 1200 words, including the urgent need to address equity globally.
Also, while #Pharmacoequity is key, it alone can't achieve health equity w/o addressing the policies that have kept certain groups w/o the resources needed to live healthily.
Also, while #Pharmacoequity is key, it alone can't achieve health equity w/o addressing the policies that have kept certain groups w/o the resources needed to live healthily.

9/ Many thanks to @walidgellad & @DusetzinaS, two of the smartest people I know studying drug policy, for helping bring my #Pharmacoequity vision to the page.
For more on our piece & another great JAMA Viewpoint out today check out our podcast convo. 👇🏾
edhub.ama-assn.org/jn-learning/au…
For more on our piece & another great JAMA Viewpoint out today check out our podcast convo. 👇🏾
edhub.ama-assn.org/jn-learning/au…

@walidgellad @DusetzinaS 10/10 We're in early stages, but really looking forward to working with @PittCP3 and the @PittTweet community to host our 1st-ever Pharmacoequity Conference here in Pittsburgh next Spring! Stay tuned!
cc @oni_blackstock @ashishkjha @DrAlethaMaybank @EbonyJHilton_MD @RheaBoydMD
cc @oni_blackstock @ashishkjha @DrAlethaMaybank @EbonyJHilton_MD @RheaBoydMD
• • •
Missing some Tweet in this thread? You can try to
force a refresh