The Chest Pain Guidelines are now released!
ahajournals.org/doi/10.1161/CI…
Top 10: CHEST PAINS
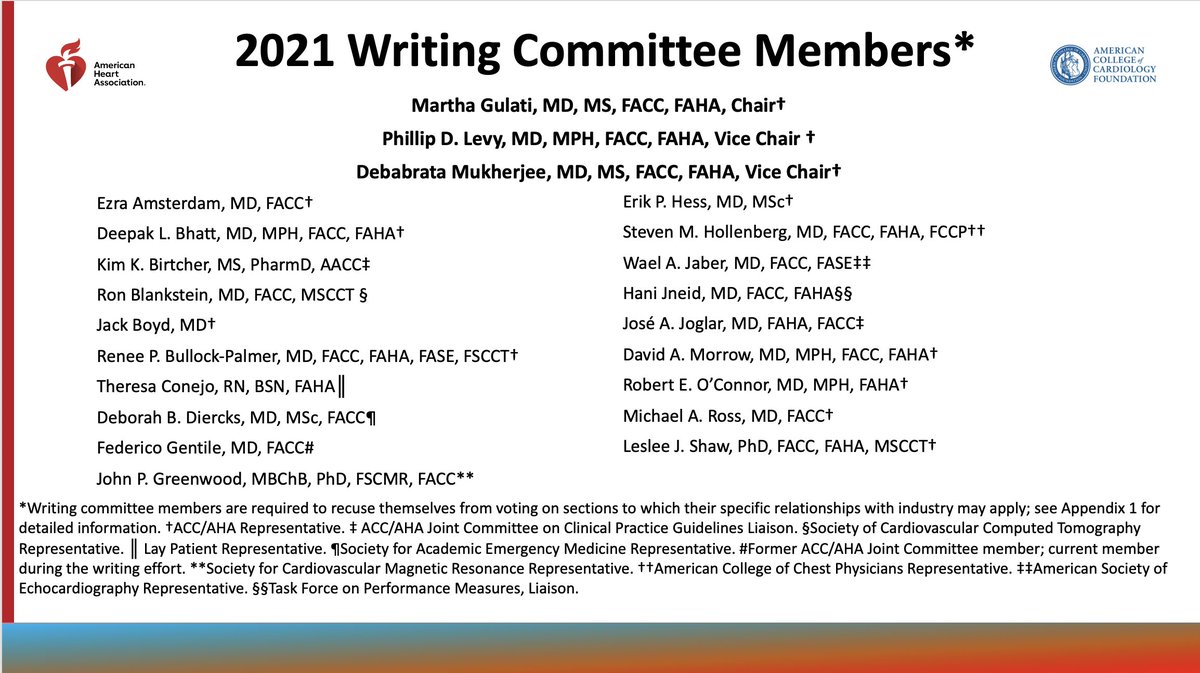
Thanks to the entire writing group and my co-cahirs: Deb Murkerjee & Phil Levy
💥First Chest Pain Guidelines @AHAScience @ACCinTouch



ahajournals.org/doi/10.1161/CI…
Top 10: CHEST PAINS
Thanks to the entire writing group and my co-cahirs: Deb Murkerjee & Phil Levy
💥First Chest Pain Guidelines @AHAScience @ACCinTouch


Top 10 messages:
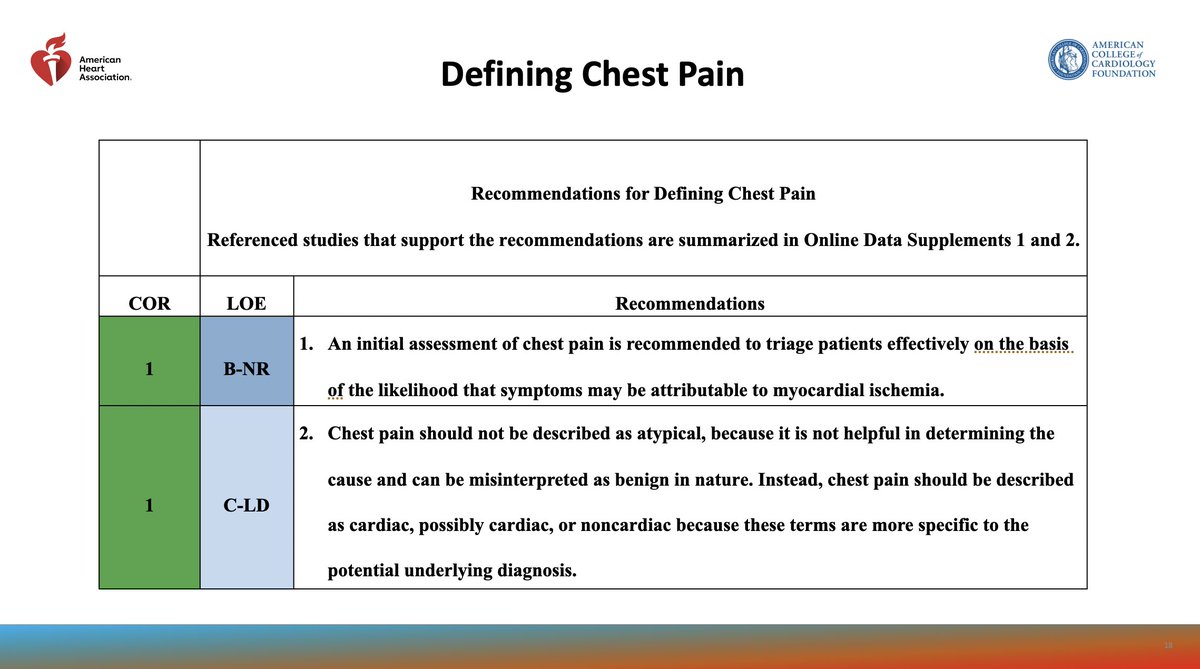
#1: Chest Pain is MORE than Pain in the chest
➡️History Matters
➡️ Assess probability of chest pain symptoms being ischemic
#1: Chest Pain is MORE than Pain in the chest
➡️History Matters
➡️ Assess probability of chest pain symptoms being ischemic

#2:High sensitivity troponin are useful and preferred biomarker
💥No more CK/CM, no more myoglobin
@HighSTEACS @MaasAngela @mmamas1973 @KTamirisaMD @iamritu @mswami001 @cardiojaydoc02 @onco_cardiology @ShelleyZieroth @fitmslax @DrToniyaSingh
💥No more CK/CM, no more myoglobin
@HighSTEACS @MaasAngela @mmamas1973 @KTamirisaMD @iamritu @mswami001 @cardiojaydoc02 @onco_cardiology @ShelleyZieroth @fitmslax @DrToniyaSingh

#3
Seek care EARLY for acute symptoms
🚑Call 9-1-1
⛔️Don't delay care in offices: send to ED if not hospital based
bit.ly/3bi6nKc
@DBelardoMD @ACCinTouch @CardioNerds @HeartOTXHeartMD @NMHheartdoc @HeartBobH
Seek care EARLY for acute symptoms
🚑Call 9-1-1
⛔️Don't delay care in offices: send to ED if not hospital based
bit.ly/3bi6nKc
@DBelardoMD @ACCinTouch @CardioNerds @HeartOTXHeartMD @NMHheartdoc @HeartBobH

#4
Share the decision making
🤝Patients are our partners
💥evidence shows when we use SDM in low risk patients , they chose less testing with no difference in outcomes
#ChestPainGuidelines
@ErikHessMD @PCORI @HeartSisters @InocaInternati1 @ShrillaB @DrNasrien @netta_doc
Share the decision making
🤝Patients are our partners
💥evidence shows when we use SDM in low risk patients , they chose less testing with no difference in outcomes
#ChestPainGuidelines
@ErikHessMD @PCORI @HeartSisters @InocaInternati1 @ShrillaB @DrNasrien @netta_doc

#5
Testing not routinely needed in low risk patients
💥One of the most important things we need to recognize!
#ChestPainGuidelines
@JoyHenningsenMD @drtaranarula @JamalRanaMD @khurramn1 @rajdoc2005 @jct_ucb @JoshuaBeckmanMD
bit.ly/3bjqqYu
Testing not routinely needed in low risk patients
💥One of the most important things we need to recognize!
#ChestPainGuidelines
@JoyHenningsenMD @drtaranarula @JamalRanaMD @khurramn1 @rajdoc2005 @jct_ucb @JoshuaBeckmanMD
bit.ly/3bjqqYu

#6
use clinical decision PATHWAYS
#CHESTPAINGUIDELINES
See pocket cards developed by @ACCinTouch here: bit.ly/3GA4kQe
@ditchhaporia @athenapoppas @DickKovacs @GatesCathy @HeartOTXHeartMD @mikevalentineMD @MinnowWalsh
use clinical decision PATHWAYS
#CHESTPAINGUIDELINES
See pocket cards developed by @ACCinTouch here: bit.ly/3GA4kQe
@ditchhaporia @athenapoppas @DickKovacs @GatesCathy @HeartOTXHeartMD @mikevalentineMD @MinnowWalsh

#7
Accompanying symptoms occur frequently in #women
As we learned from the High-STEACS group, HERMES and VIRGO, what is different between men & women is that women have more accompanying symptoms. But 90% of women do report chest pain
@lesleejshaw @Drroxmehran @SharonneHayes
Accompanying symptoms occur frequently in #women
As we learned from the High-STEACS group, HERMES and VIRGO, what is different between men & women is that women have more accompanying symptoms. But 90% of women do report chest pain
@lesleejshaw @Drroxmehran @SharonneHayes

#8
Identify patients who are most likely to benefit from further testing
💥Chose the right patient
💥Chose the right test
#ChestPainGuidelines
Flib book here from @ACCinTouch : bit.ly/3pOzdu6
Identify patients who are most likely to benefit from further testing
💥Chose the right patient
💥Chose the right test
#ChestPainGuidelines
Flib book here from @ACCinTouch : bit.ly/3pOzdu6

#9
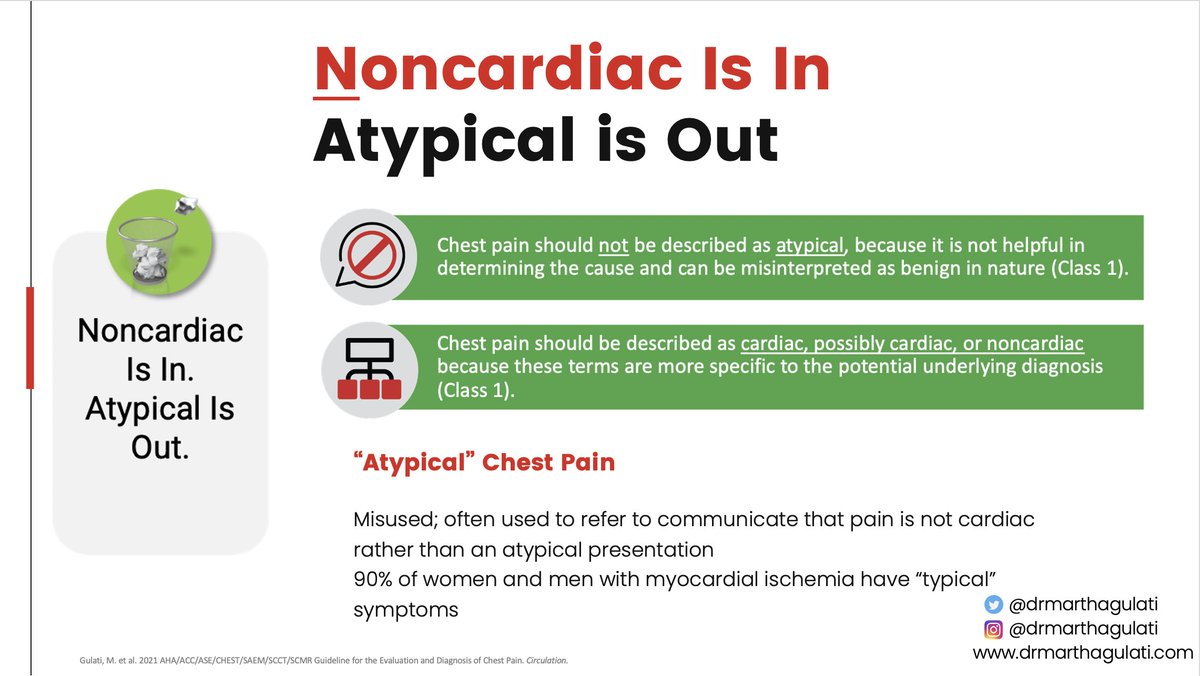
Non cardiac is in
Atypical is Out
💥The work "atypical" has been misused to represent non-cardiac. Let's not use this anymore. #wordsmatter
#ChestPainGuidelines
@HeartSisters @InocaInternati1 @heart_spasms @DrJMieres @dranulala @HeartDocSharon
Non cardiac is in
Atypical is Out
💥The work "atypical" has been misused to represent non-cardiac. Let's not use this anymore. #wordsmatter
#ChestPainGuidelines
@HeartSisters @InocaInternati1 @heart_spasms @DrJMieres @dranulala @HeartDocSharon
#10
Structured risk assessment should be used
#ChestPainGuidelines
Use this link for all tools by @ACCinTouch (Guideline Hub!): bit.ly/3CspzRj
Structured risk assessment should be used
#ChestPainGuidelines
Use this link for all tools by @ACCinTouch (Guideline Hub!): bit.ly/3CspzRj

From @CardioSmart for our patients we have a #CHESTPAIN hub with a wonderful infographic (one of the last things I worked on as EIC!) from this link: bit.ly/3CoXwSJ
and
the hub for patients: bit.ly/3GqfwyJ
Thanks @mpob & @ACCinTouch for doing this!
and
the hub for patients: bit.ly/3GqfwyJ
Thanks @mpob & @ACCinTouch for doing this!

• • •
Missing some Tweet in this thread? You can try to
force a refresh