Why are thiazides effective in augmenting natriuresis when added to loops?
We all know that exposure to loops➡️increase in NCC channels in the distal tubule
BUT there's more
Did you know that there's a mechanism for thiazide sensitive NaCl reabsorption in the collecting duct?

We all know that exposure to loops➡️increase in NCC channels in the distal tubule
BUT there's more
Did you know that there's a mechanism for thiazide sensitive NaCl reabsorption in the collecting duct?


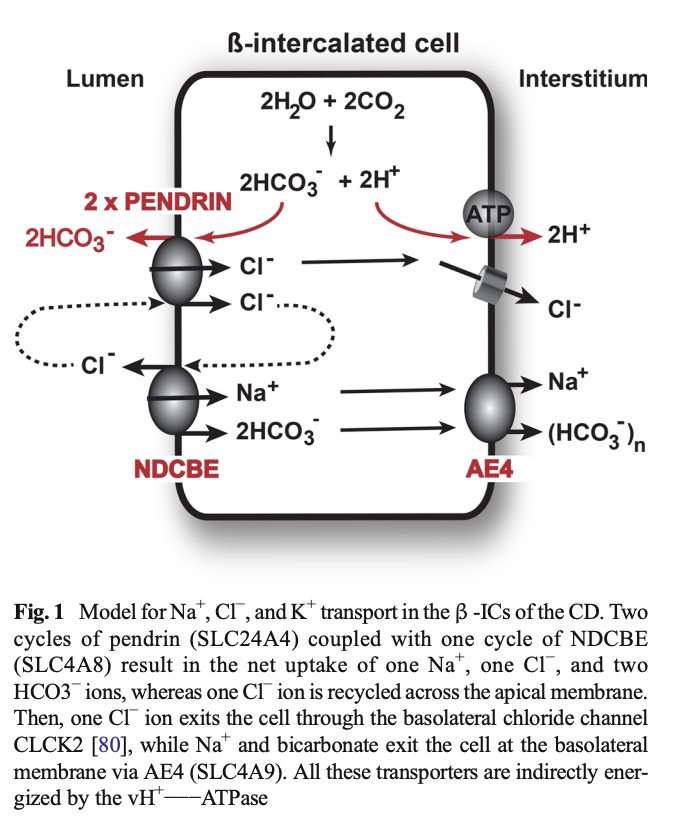
Electroneutral NaCl absorption can also occur in the collecting duct through the parallel action of pendrin and NDCBE (Na-dependent Cl/HCO3 exchanger) which is upregulated by Ang II and mineralocorticoids (when Ang II present)
2 cycles of pendrin = 2HCO3- to the lumen for 2Cl-. 1 Cl- is recycled to NDCBE resulting in net reabsorption of 1 NaCl and 2 HCO3- (Cl- through CLCK2 and Na and HCO3- through AE4 in the basolateral membrane)
The whole mechanism appears to be thiazide sensitive
The whole mechanism appears to be thiazide sensitive
Maybe pendrin will be the target for the next diuretic??
Good articles regarding the above here:
pubmed.ncbi.nlm.nih.gov/20389022/
and here:
pubmed.ncbi.nlm.nih.gov/25794953/
#diuresisjedi
Good articles regarding the above here:
pubmed.ncbi.nlm.nih.gov/20389022/
and here:
pubmed.ncbi.nlm.nih.gov/25794953/
#diuresisjedi
• • •
Missing some Tweet in this thread? You can try to
force a refresh