
1/ As famous @WakeForest professor Maya Angelou said, “When people show you who they are believe them” —stunning reveals here—Former @UHC exec says company would only pay surprise bills after complaints….beckershospitalreview.com/payer-issues/f…? @drdanchoi utm_source=twitter&utm_medium=social 



2/ @Reese_Tassey @813JAFERD @sonodoc99 @fuzzymittens @amychomd @ercoderguy @MarilynHeineMD @Valleus556 @mass_marion @A4Horg @CRCook1978 @ZachJonesForTX @ASAGrassroots @EmergencyDocs @RadiologyACR @AmerMedicalAssn @ahahospitals @teamhealth @EDPMA @KatieOrrico @GrassrootsEM
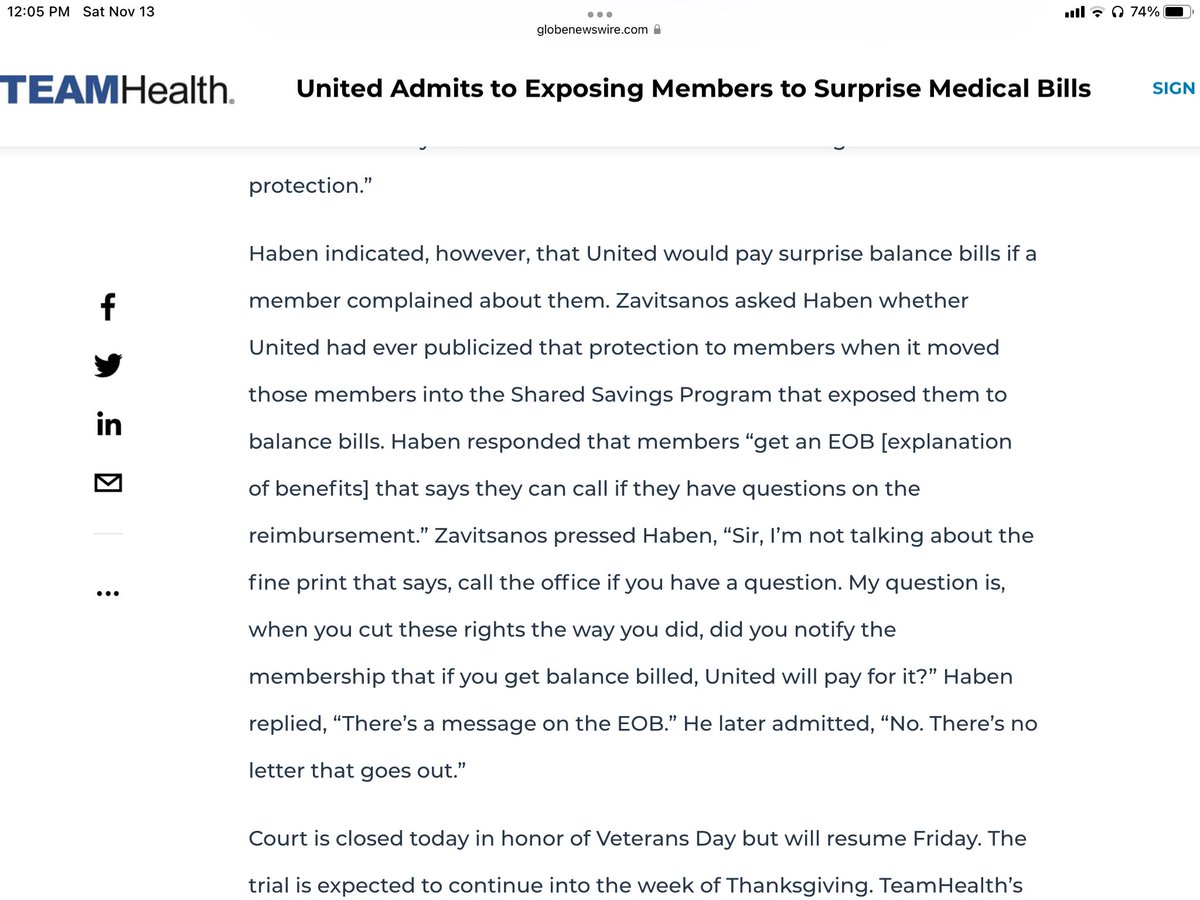
3/ So the former senior exec. for @UHC admits that it did not inform members in writing via letter that #UnitedHealth would reimburse out of network bills, instead it was buried in the fine print of the #EOB to the Pt. & Pts. had to ask UHC to pay. 
4/More conflicts of interest (COI) evidence mounting @NEJM @zackcooperYale as testimony shows how @UHC planned to get specific physician group names in front of the professor & more importantly the “data” to support that narrative—don’t be surprised as #UHC scammed w/ Ingenix too
• • •
Missing some Tweet in this thread? You can try to
force a refresh




