1/ It is near the end of your time on inpatient service and it has been BUSY!
Spirits are high, but folks are tired.
You want to make sure rounds are high-yield, but how to focus their energy?
Welcome back #MedTwitter & #MedEd for another #TweetorialTuesday from @MedEdTwagTeam!
Spirits are high, but folks are tired.
You want to make sure rounds are high-yield, but how to focus their energy?
Welcome back #MedTwitter & #MedEd for another #TweetorialTuesday from @MedEdTwagTeam!

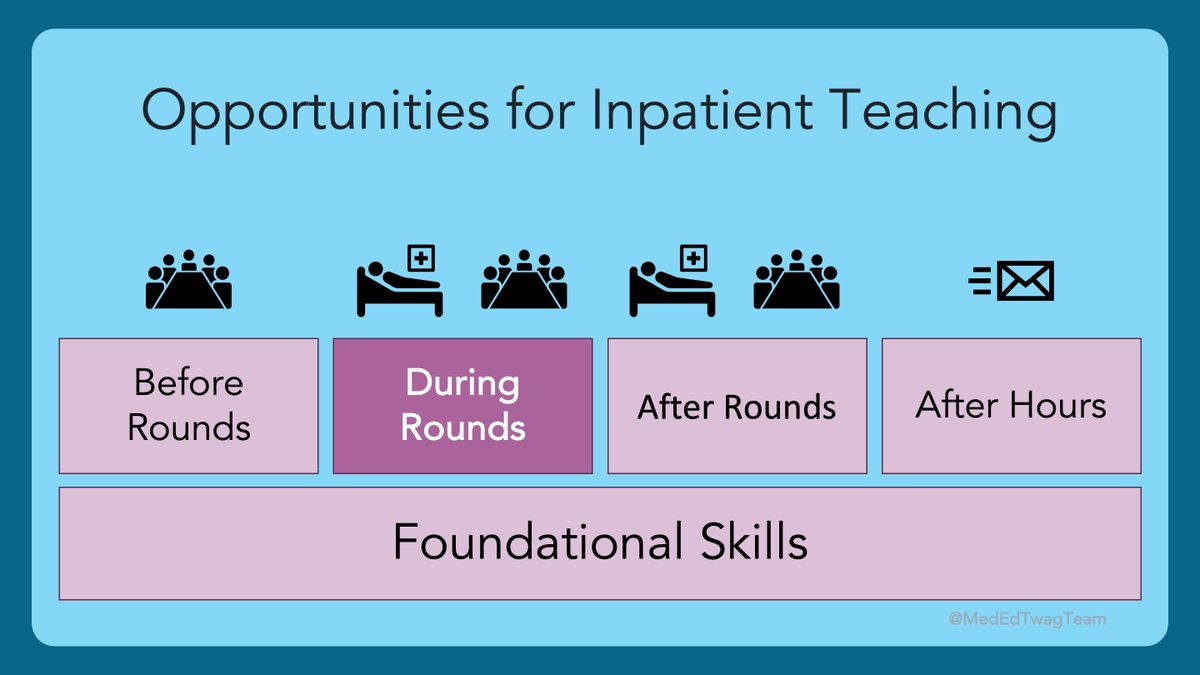
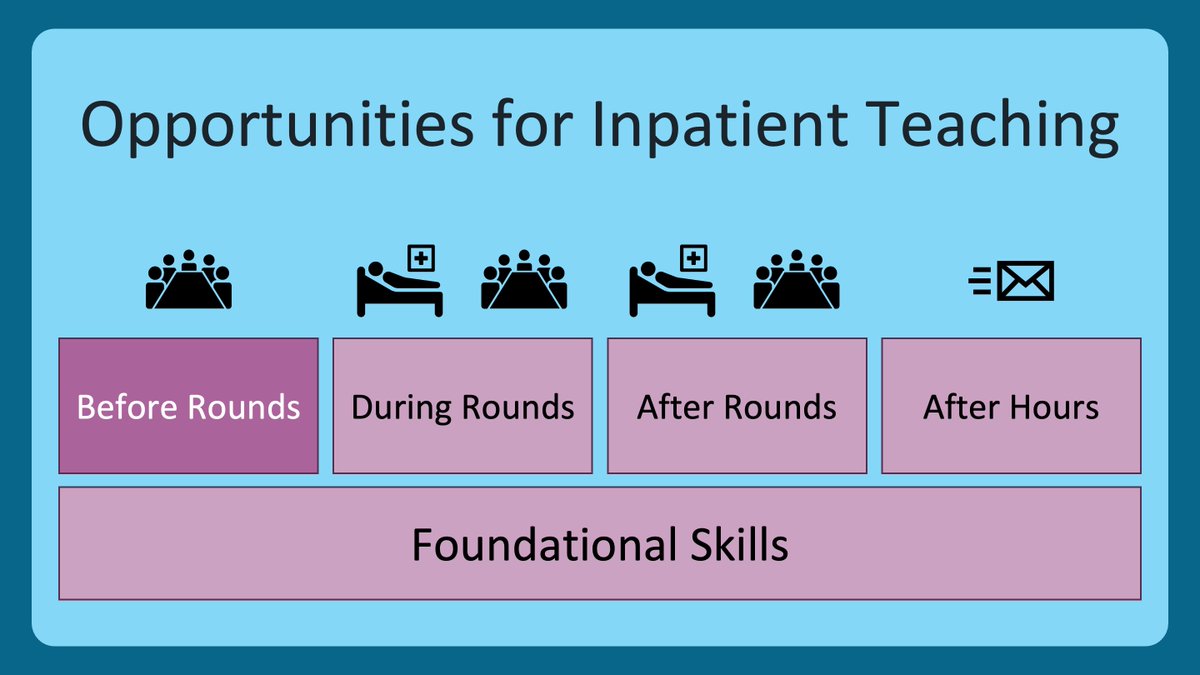
2/ This week, I will share tips on how to use questions to get ”the wheels turning” for your learners before rounds.
In just a few minutes, this focuses energy, engages team members in the cases they may not be following, and enhances bedside learning for everyone.
In just a few minutes, this focuses energy, engages team members in the cases they may not be following, and enhances bedside learning for everyone.
3/ Today’s 🧵 harkens back to one I posted about ”prediction questions”.
Inspiration: #SmallLearning from @LangOnCourse. It is tremendous, with a lot of useful ideas that can be applied in the classroom or clinical setting. FYI - 2nd ed just came out.
Inspiration: #SmallLearning from @LangOnCourse. It is tremendous, with a lot of useful ideas that can be applied in the classroom or clinical setting. FYI - 2nd ed just came out.
https://twitter.com/GStetsonMD/status/1402291340092788736
4/ @LangOnCourse provides a great analogy about the power of prediction: "[Predictive exercises] till the soil of your students minds and prepare a fertile ground for the learning that will follow." 
5/ So, what is the science here?
Generating a prediction does a few things to improve learning from an emotional & cognitive standpoint:
Generating a prediction does a few things to improve learning from an emotional & cognitive standpoint:

6/ So how is it done? Here are some examples of scenarios and questions that can be asked about patients on a team that can prep your team for learning: 

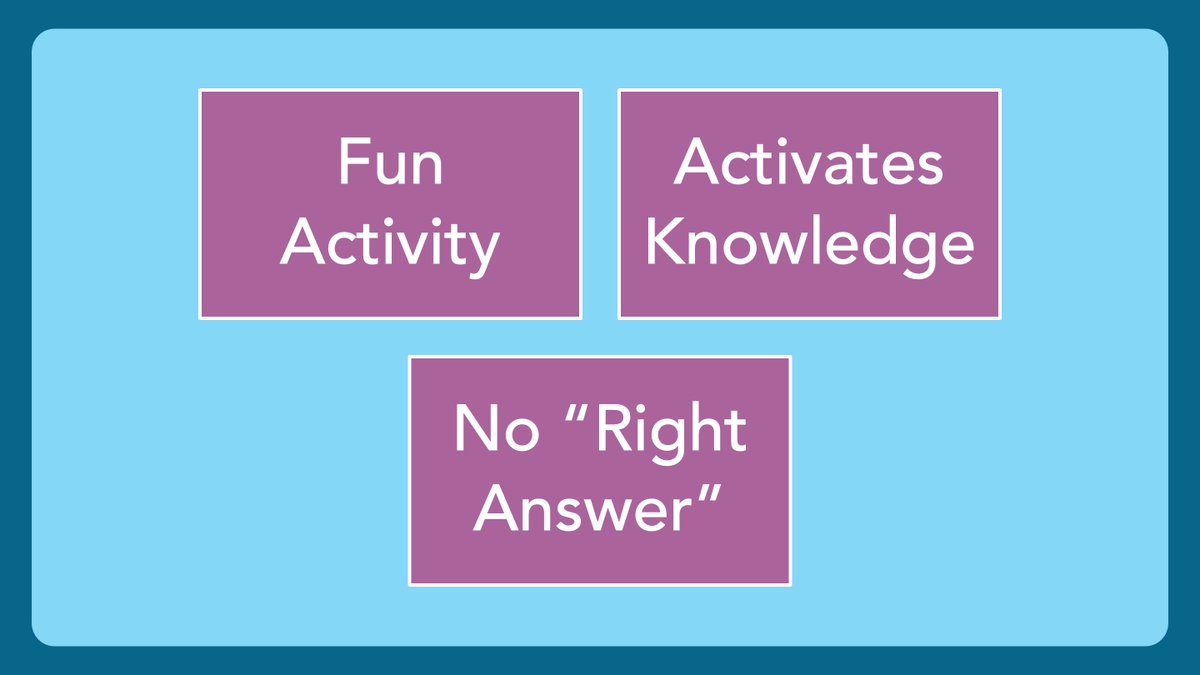
7/ What makes a good prediction question:
✅ It is posed as a fun activity to get people thinking
✅ It activates previous knowledge
✅ There is no ”right answer”. You all will discover the answer later when you see the patient, the consultant weighs in, or some result returns.
✅ It is posed as a fun activity to get people thinking
✅ It activates previous knowledge
✅ There is no ”right answer”. You all will discover the answer later when you see the patient, the consultant weighs in, or some result returns.
8/ This is a GREAT way to get all learners involved.
The primary provider has been thinking deeply about the patient, while others may not know much about them.
This helps focus all learners before meeting a new patient & prepares them to incorporate new information.
The primary provider has been thinking deeply about the patient, while others may not know much about them.
This helps focus all learners before meeting a new patient & prepares them to incorporate new information.
9/ After a prediction is made, however, it is important to discover the right answer ASAP.
One cannot let an incorrect prediction linger too long, as that risks cementing that prediction as “truth.”
One cannot let an incorrect prediction linger too long, as that risks cementing that prediction as “truth.”
10/ After you discover the truth, reflecting on your predictions is key to learning:
❓ Were you right? Wrong? Somewhere in between? Why?
❓ Did the patient’s presentation differ from a typical presentation? Why?
❓ Are there assumptions you made that must be challenged?
❓ Were you right? Wrong? Somewhere in between? Why?
❓ Did the patient’s presentation differ from a typical presentation? Why?
❓ Are there assumptions you made that must be challenged?
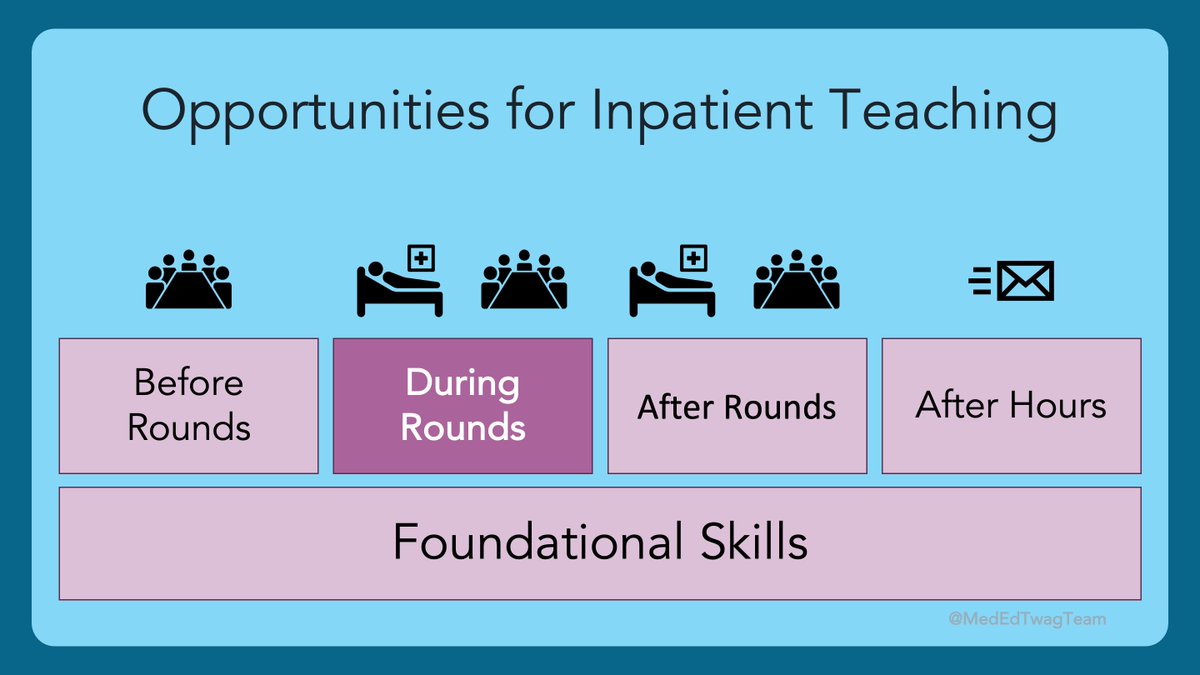
11/ This process is summed up with three key ideas:
🔑 Prediction (before rounds)
🔑 Exposure (getting the answer, during or after rounds)
🔑 Reflection (best as a group, during or after rounds)
🔑 Prediction (before rounds)
🔑 Exposure (getting the answer, during or after rounds)
🔑 Reflection (best as a group, during or after rounds)
12/ Are there other ways that you all get your learners ready to learn at the beginning of a clinical day?
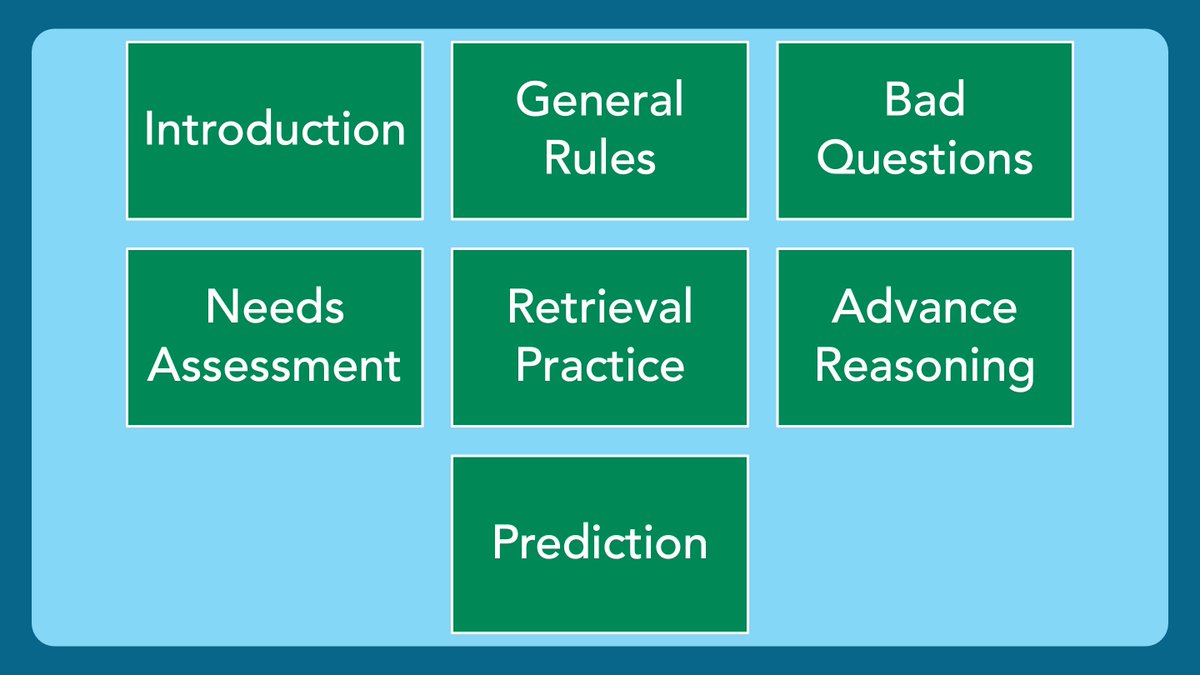
Here’s a summary of how prediction questions can be used to prime learning and why it works.
Here’s a summary of how prediction questions can be used to prime learning and why it works.

13/ Thanks for joining us today!
The @MedEdTwagTeam is taking a break for a few weeks to spend some holiday QT with our families. For those who celebrate, we hope you are able to do the same!
Thanks #MedEd & #MedTwitter for all the support & engagement! Tweet you in 2022!
The @MedEdTwagTeam is taking a break for a few weeks to spend some holiday QT with our families. For those who celebrate, we hope you are able to do the same!
Thanks #MedEd & #MedTwitter for all the support & engagement! Tweet you in 2022!

• • •
Missing some Tweet in this thread? You can try to
force a refresh