Nice mask study ~consistent w/ prev. results.
pnas.org/content/118/49…
"... face masks sign. reduce the risk of SARS-CoV-2 infection compared to social distancing. We find a very low risk of inf. when everyone wears a face mask, even if it doesn’t fit perfectly on the face." 1/🧵
pnas.org/content/118/49…
"... face masks sign. reduce the risk of SARS-CoV-2 infection compared to social distancing. We find a very low risk of inf. when everyone wears a face mask, even if it doesn’t fit perfectly on the face." 1/🧵

2/ The authors perform "upper bound" analyses to get around complexities in modeling risk.
"We conclude that wearing appropriate masks in the community provides excellent protection for others and oneself, and makes social distancing less important."
pnas.org/content/118/49…
"We conclude that wearing appropriate masks in the community provides excellent protection for others and oneself, and makes social distancing less important."
pnas.org/content/118/49…
3/ I especially like this overview schematic comparing FFP2 (~N95) to surgical mask usage based on combos between two people.
Consistent with the old refrain "any mask is better than no mask, but masks with better fit & filtration protect much more."
Consistent with the old refrain "any mask is better than no mask, but masks with better fit & filtration protect much more."

4/ With no masks & only distancing (3 m), 90% risk of infection.
"When both wear a surgical mask, while the infectious is speaking, the very conservative upper bound remains below 30% after 1 h, but, when both wear a well-fitting FFP2 mask, it is 0.4%."
pnas.org/content/118/49…
"When both wear a surgical mask, while the infectious is speaking, the very conservative upper bound remains below 30% after 1 h, but, when both wear a well-fitting FFP2 mask, it is 0.4%."
pnas.org/content/118/49…

5/ They also looked at the effect of fit on TIL (total inward leakage).
"By simply adjusting the mask nosepiece to the nose, case (ii), the mask's TIL is improved by a factor of 4.3 for the smallest particles and by a factor of 7.5 for 3 micron particles"
pnas.org/content/118/49…
"By simply adjusting the mask nosepiece to the nose, case (ii), the mask's TIL is improved by a factor of 4.3 for the smallest particles and by a factor of 7.5 for 3 micron particles"
pnas.org/content/118/49…

6/ "The surgical mask, however, is associated with the highest total inward leakage, with the maximum value being in excess of 70% occurring for the smallest particle size."
"Wearing an additional surgical mask on top of the adjusted FFP2 masks, case (iii)" didn't add much here.
"Wearing an additional surgical mask on top of the adjusted FFP2 masks, case (iii)" didn't add much here.

7/ They mention that surgical masks have great filtration quality & increased infection risk compared to FFP2 (N95) masks is due to leakage.
Good news: Note also in C here that risk can be lowered substantially even if only susceptible person is wearing a mask (lowest if FFP2).
Good news: Note also in C here that risk can be lowered substantially even if only susceptible person is wearing a mask (lowest if FFP2).
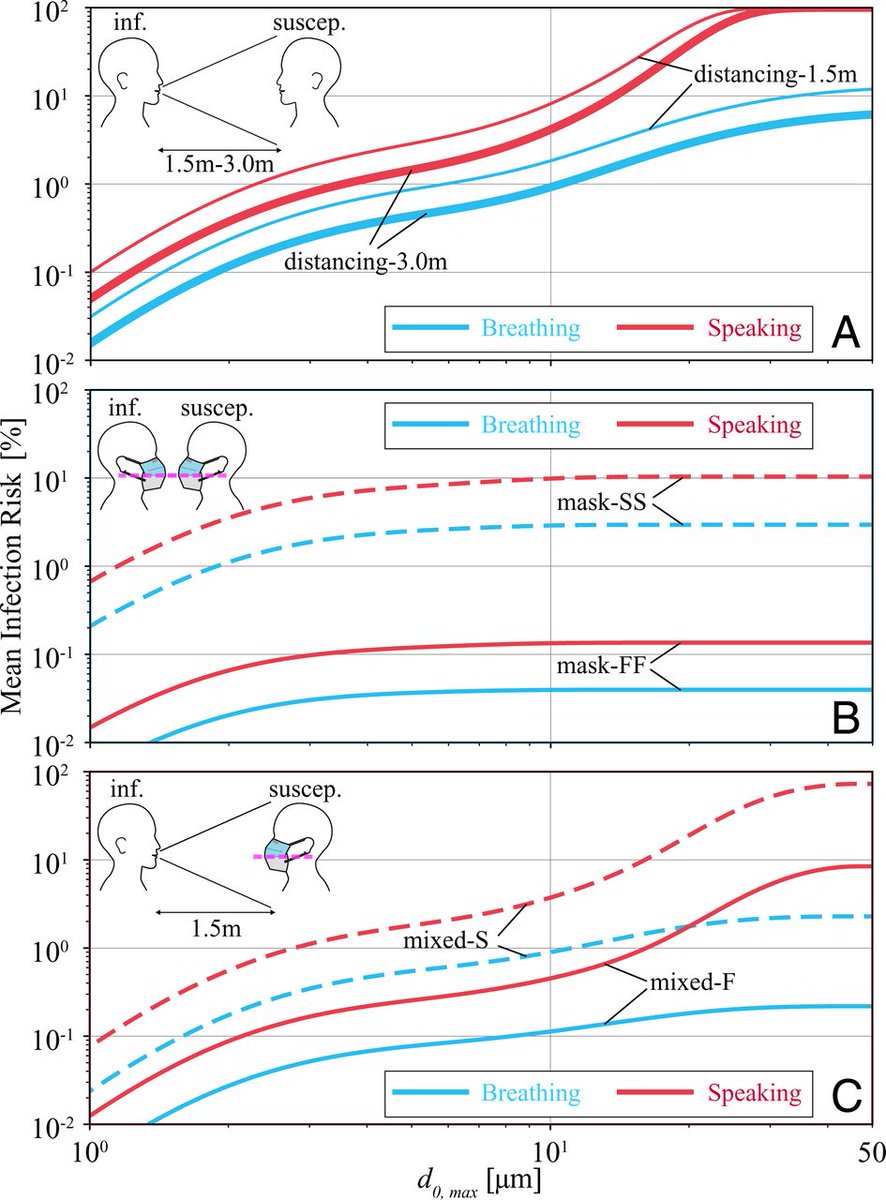
8/ Ultimately, they calculate estimated infection risk as a function of exposure time under several combos of surgical or FFP2 masks, both during breathing and speaking (worse).
I would argue that the exact y-scale values are less important than the trends with time & mask type.
I would argue that the exact y-scale values are less important than the trends with time & mask type.

9/ The study is really nice, and they do a good job of calculating through "upper bounds" of assumed and calculated risk factors to limit issues with complex uncertainties.
The results are also qualitatively consistent with previous estimates.
The results are also qualitatively consistent with previous estimates.
https://twitter.com/akm5376/status/1425014228159717390
10/ As their study suggests, surgical masks reduce aerosol inhalation risk, and FFP2/N95 (& elastomeric respirators) do dramatically better job still - based primarily on the differences in FIT.
https://twitter.com/HuffmanLabDU/status/1357816943290449920?s=20
11/ The paper is really useful to put estimated bounds on risk reduction using different masks: pnas.org/content/118/49…
But ultimately, this old/nice graphic from @DrEmilySomers tells a simple summary ⬇️. And the #BetterMask you wear, even lower the risk.

But ultimately, this old/nice graphic from @DrEmilySomers tells a simple summary ⬇️. And the #BetterMask you wear, even lower the risk.

12/ And from a practical perspective, many places to find high-quality N95 (US), FFP2 (Europe), & KF94-rated masks/respirators.
See links in thread below to buy from the non-profit @projectn95 (in US) or others in Canada & to see mask data from @masknerd.
See links in thread below to buy from the non-profit @projectn95 (in US) or others in Canada & to see mask data from @masknerd.
https://twitter.com/HuffmanLabDU/status/1466188864989515782
13/ Another practical point:
N95 masks don't have to be expensive. They can be ~$1/each: shop.projectn95.org/all/.
Expensive if disposed after every use, but can be reused for a while. Use, set aside for 1-2 days, rotate back until straps break or dirty.
N95 masks don't have to be expensive. They can be ~$1/each: shop.projectn95.org/all/.
Expensive if disposed after every use, but can be reused for a while. Use, set aside for 1-2 days, rotate back until straps break or dirty.
https://twitter.com/HuffmanLabDU/status/1357818178689069057
14/ #Elastomeric respirators can also be an excellent way to get N95+/FFP2+ level filtration in a reusable form that seals well (gel or rubber) & that can be more comfortable than others.
@PPEtoheros & e.g.:
cleanaircrew.org/elastomeric-re…
@PPEtoheros & e.g.:
https://twitter.com/LazarusLong13/status/1425908588954853382
cleanaircrew.org/elastomeric-re…
https://twitter.com/Amal4Solutions/status/1435661435653087235
• • •
Missing some Tweet in this thread? You can try to
force a refresh



















