New analysis in @NEJM today with coauthors @McGarryBE @ashdgandhi @DavidCGrabowski
Vaccine mandates continue to be controversial, including in nursing homes. What are the stakes exactly?
The results are sobering, to say the least ...
nejm.org/doi/full/10.10…

Vaccine mandates continue to be controversial, including in nursing homes. What are the stakes exactly?
The results are sobering, to say the least ...
nejm.org/doi/full/10.10…

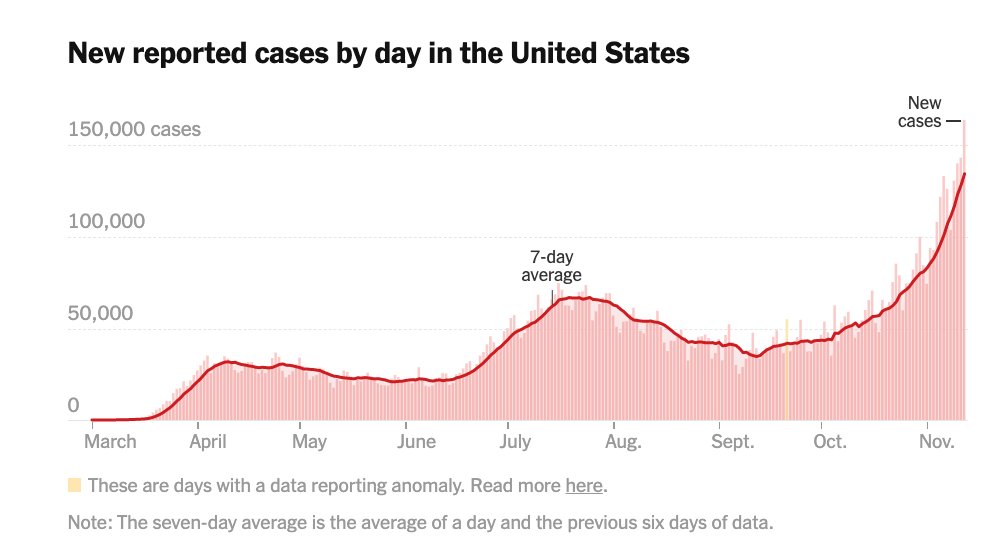
@NEJM @McGarryBE @ashdgandhi @DavidCGrabowski From June-Aug 2021, we compared resident and staff infection + mortality rates between 12,000 homes with the lowest staff vaccination rates (~30%) vs. highest (~80%).
In the least vaccinated homes:
+132% COVID cases in residents
+58% staff cases
+195% resident mortality
yikes
In the least vaccinated homes:
+132% COVID cases in residents
+58% staff cases
+195% resident mortality
yikes

@NEJM @McGarryBE @ashdgandhi @DavidCGrabowski Over an 8 week period, if all nursing homes were magically raised to the highest staff vaccination levels nationally (~80%), we would have:
4,775 fewer resident cases
7,501 fewer staff cases
703 fewer resident deaths (nearly 50% of all deaths)
4,775 fewer resident cases
7,501 fewer staff cases
703 fewer resident deaths (nearly 50% of all deaths)

@NEJM @McGarryBE @ashdgandhi @DavidCGrabowski There was no difference in areas with low COVID-19 prevalence, underscoring that vaccination itself is probably the key difference here (rather than other confounding)
This should not be a controversial thing to say, but COVID-19 vaccination saves lives. Mandates = life saving.
This should not be a controversial thing to say, but COVID-19 vaccination saves lives. Mandates = life saving.
• • •
Missing some Tweet in this thread? You can try to
force a refresh