1/ A big part of understanding the relationship between COVID cases and mortality is understanding the age structure of the waves
I've been looking at NYC "Respiratory" syndrome for ED visits (I was a member of the group that pioneered its use for public health 20 years ago)
I've been looking at NYC "Respiratory" syndrome for ED visits (I was a member of the group that pioneered its use for public health 20 years ago)
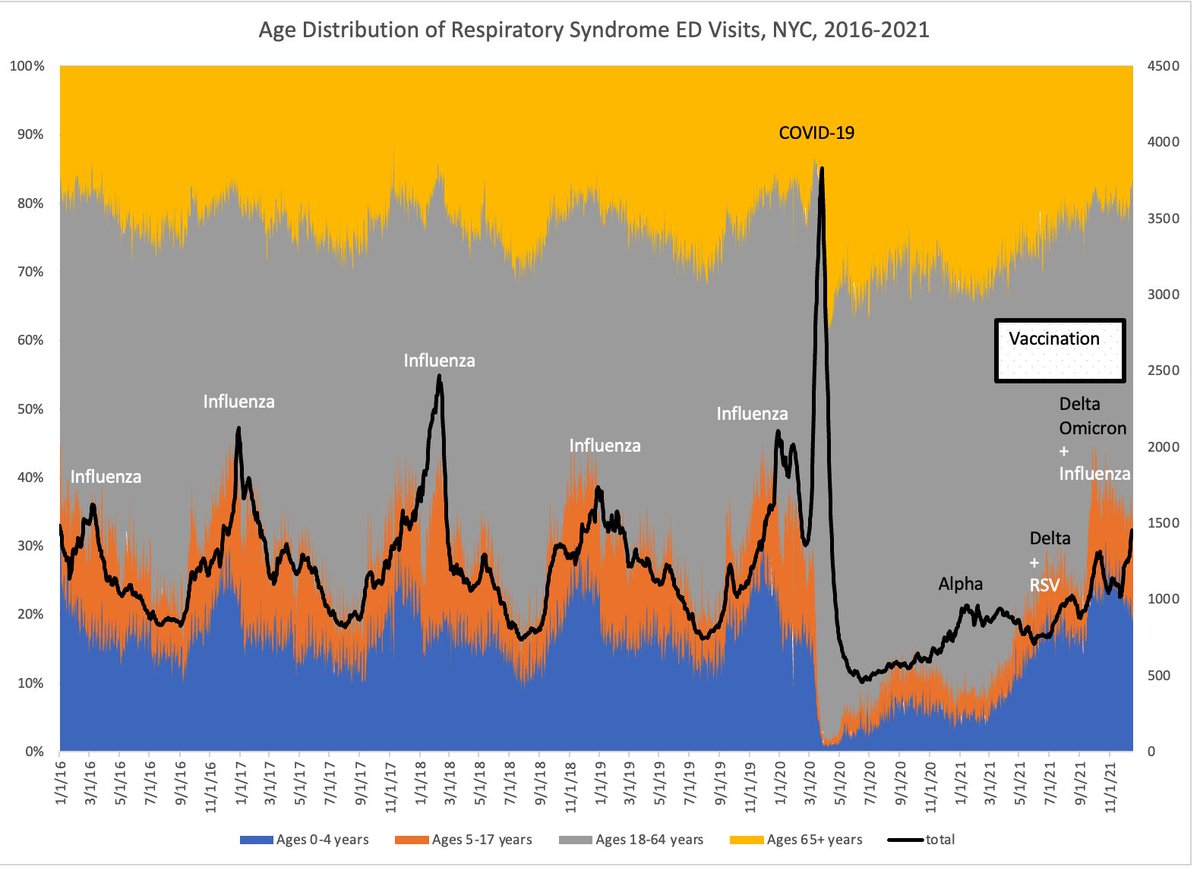
2/ During prior influenza seasons, NYC would have up to 1,000 extra emergency department visits a day, much of the increase driven by babies and children (low prior immunity). Their share of ED visits would increase from ~20% to 40%
COVID19 was a completely different story
COVID19 was a completely different story
3/ Every day the number of ED visits rose higher. I remember seeing the first break in the relentless increase, and barely daring to believe that we had reached a peak. It was March 28. There were an extra 3,000 ED visits that day.
But even worse, they were almost adults.
But even worse, they were almost adults.

4/ Older people in March 2020 had no prior immunity to COVID19 and we paid the price. Hospitals were completely overwhelmed. And then the morgues.
The Alpha wave caused a much smaller increase (and again the proportion of adults went up)
But pretty soon vaccinations kicked in
The Alpha wave caused a much smaller increase (and again the proportion of adults went up)
But pretty soon vaccinations kicked in
5/ During the summer lull and the early fall Delta wave you could literally see the proportion of elderly among the Respiratory ED group shrinking as vaccines did their magic.
In September, with social distancing fatigue, RSV came roaring back among children, as Delta simmered
In September, with social distancing fatigue, RSV came roaring back among children, as Delta simmered

6/ Which brings us to December.
I think we have 3 separate things going on.
Influenza is now rising
Delta is continuing
Omicron is kicking in.
We are not seeing a shift in ED visits towards the elderly, and that gives me great hope that the vaccines are holding
I think we have 3 separate things going on.
Influenza is now rising
Delta is continuing
Omicron is kicking in.
We are not seeing a shift in ED visits towards the elderly, and that gives me great hope that the vaccines are holding

7/ There has undoubtedly been a bump up in Respiratory ED visits in NYC (it would be shocking if there weren't, in the midst of the greatest number of new cases diagnosed ever)
But it's on the order of 500 extra visits a day.
Historically speaking, that's not yet unusual

But it's on the order of 500 extra visits a day.
Historically speaking, that's not yet unusual


8/ And from what I can tell so far, the vast majority of those respiratory (and ILI, and COVID-like) ED visits are not getting admitted
There were a total of 200 pneumonia and influenza admissions (103 COVID+) on 12/19, which is only 36 cases above seasonal baseline
👍 🙏 🤞
There were a total of 200 pneumonia and influenza admissions (103 COVID+) on 12/19, which is only 36 cases above seasonal baseline
👍 🙏 🤞

9/ If you want to learn the backstory on the development of these syndromic surveillance systems (for bioterrorism, no less), can read @chrissyfarr excellent piece and my commentary here
https://twitter.com/Farzad_MD/status/1246439633715695616?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh