1/ Let's do an exercise together:
We've often heard people say something like "this innovative new service/company is good for patients and saves money, but there's no business model for it/ current reimbursement doesn't support it"
Step 1: Let's generate examples:
We've often heard people say something like "this innovative new service/company is good for patients and saves money, but there's no business model for it/ current reimbursement doesn't support it"
Step 1: Let's generate examples:

2/ I'll start.
But this is a group exercise, I need your nominations. Please try to give suggestions with some evidence behind them
*Advanced Care Planning
*Hospital at home
*Diabetes prevention program
*"SDOH" care navigation
(Used to be, telehealth)
But this is a group exercise, I need your nominations. Please try to give suggestions with some evidence behind them
*Advanced Care Planning
*Hospital at home
*Diabetes prevention program
*"SDOH" care navigation
(Used to be, telehealth)
3/ great work, tweeple
Clearly no shortage of ideas (with varying level of evidence) for things that could save money and be good for patients
The view espoused by many (including yours truly) has been that these services will flourish under value-based care
But not that easy
Clearly no shortage of ideas (with varying level of evidence) for things that could save money and be good for patients
The view espoused by many (including yours truly) has been that these services will flourish under value-based care
But not that easy
4/ How do you actually make a business out of these solutions?
You go to health plans and say:
a) this will save you money. trust me. but pay me now so I can pay my staff.
b) I will do it for free, pay me if your costs are actually lower than expected
Which one do you choose?
You go to health plans and say:
a) this will save you money. trust me. but pay me now so I can pay my staff.
b) I will do it for free, pay me if your costs are actually lower than expected
Which one do you choose?
5/ The problem with a) is convincing the health plan that your elderly loneliness service is going to actually save them money
Given uncertainty the negotiations will be lengthy, you will have little leverage, and they will heavily discount what they pay you (either FFS or pmpm)
Given uncertainty the negotiations will be lengthy, you will have little leverage, and they will heavily discount what they pay you (either FFS or pmpm)

6/ ..and you're at the mercy of the plan dropping you or negotiating (OK, "negotiating") lower rates each year.
And you can't blame them. with all these solutions they must feel like they are being nibbled at by a swarm of ... umm... piranhas?
And you can't blame them. with all these solutions they must feel like they are being nibbled at by a swarm of ... umm... piranhas?
https://twitter.com/CraigJoseph/status/1449809613981995012?s=20
7/ The other problem with paying "fee-for-service" for theoretically value-creating stuff is that it destroys the incentive to finely target the intervention to those for whom it makes the biggest difference
In fact, it might be easiest to deliver the service to the wrong people
In fact, it might be easiest to deliver the service to the wrong people
8/ This is what has arguably happened with most of the well-intentioned efforts by @CMSGov to create "good FFS" codes
The NNT for preventing a readmission with Transitional Care Management is only 7.7 for highest impactable quartile, over 100 for lowest.
But they pay the same
The NNT for preventing a readmission with Transitional Care Management is only 7.7 for highest impactable quartile, over 100 for lowest.
But they pay the same
9/ Option b then-
Let's do shared savings!
You will have to really really have confidence that you will create savings. That's honestly not a bad thing. There are lots of great services suggested in the replies.
But how many would you put your own skin in the game for?
Let's do shared savings!
You will have to really really have confidence that you will create savings. That's honestly not a bad thing. There are lots of great services suggested in the replies.
But how many would you put your own skin in the game for?
10/ But unlike ACOs (total cost of care for large population), many of these services don't have standardized contract templates for calculation of benchmarks and trends, and quality gates.
And it's hard to get to the numbers you need to reduce random variation in costs
also..
And it's hard to get to the numbers you need to reduce random variation in costs
also..
11/ Health plans may not want to have to integrate, arbitrate, and/or consolidate across multiple value-based services, especially when multiple different solutions are being offered, and each one might want to take credit for the savings.
https://twitter.com/sacjai/status/1451218223253307392?s=20
12/ The final challenge for our peer-based care giver support entrepreneur is going to be engaging w the member with "I'm calling from your health plan"
Given 1,000 members who meet eligibility requirements, how many will pick up phone, agree, engage?
Usually~10%-15% Often ~5%
Given 1,000 members who meet eligibility requirements, how many will pick up phone, agree, engage?
Usually~10%-15% Often ~5%
13/ A low engagement rate drives up costs, reduces revenue, and increases the noise in value-based deals.
The savings analysis is unlikely to find savings if you only engaged 10% of the "intention to treat" population
(most plans understand selection bias by now)
The savings analysis is unlikely to find savings if you only engaged 10% of the "intention to treat" population
(most plans understand selection bias by now)
14/ So what's the end-game then?
Payers will gravitate towards companies that offer comprehensive solutions
I think it's inevitable that a lot of these companies will not survive as stand-alone businesses- you are either a consolidator or consolidated
Payers will gravitate towards companies that offer comprehensive solutions
I think it's inevitable that a lot of these companies will not survive as stand-alone businesses- you are either a consolidator or consolidated
https://twitter.com/healthcareandy/status/1442166665328791562?s=20
15/ Who will the consolidators be?
A. Members of the class
@TeladocHealth /@Livongo were the first to realize this dynamic.
@grandroundsinc / @drondemand
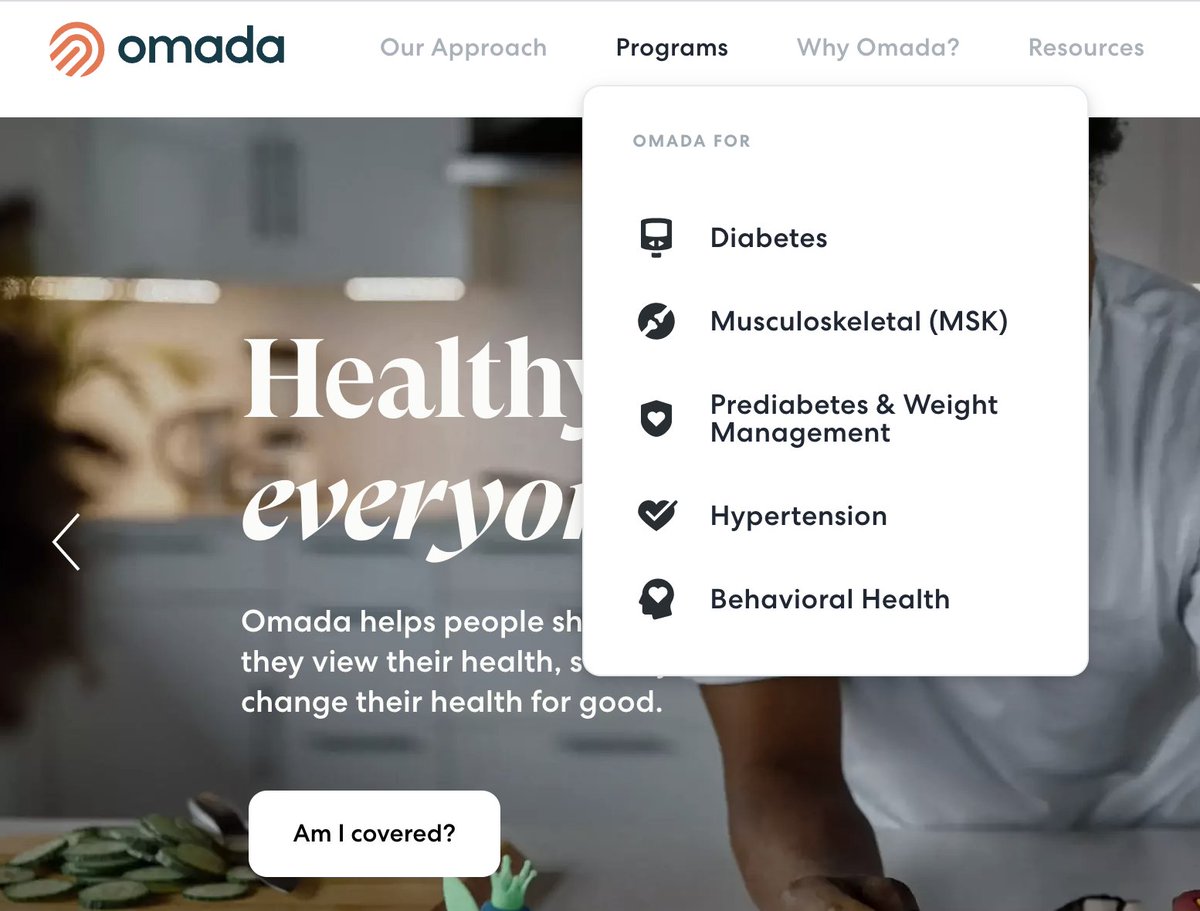
@omadahealth started as diabetes, bought @physera now look at what they cover, with more surely to come.
A. Members of the class
@TeladocHealth /@Livongo were the first to realize this dynamic.
@grandroundsinc / @drondemand
@omadahealth started as diabetes, bought @physera now look at what they cover, with more surely to come.
16/ It could be that health plans themselves try to consolidate the "best in class" (or "best that I can buy").
They haven't been successful so far. It's possible that there's selection bias at work.
Companies that know they're onto something big may not want to sell to a plan
They haven't been successful so far. It's possible that there's selection bias at work.
Companies that know they're onto something big may not want to sell to a plan
17. But I think the most likely candidates for integrating, arbitrating, and/or consolidating these solutions are primary care-centered companies that are already taking full cost and quality accountability
https://twitter.com/Farzad_MD/status/1451251612127842306?s=20
18. Why?
Build, Buy, or Buy
*They can capture the full value of savings created
*They can capture both clinical and claims (through risk contracts) data to effectively target interventions for highest ROI
*They can increase engagement through warm handoffs from aligned PCPs.
Build, Buy, or Buy
*They can capture the full value of savings created
*They can capture both clinical and claims (through risk contracts) data to effectively target interventions for highest ROI
*They can increase engagement through warm handoffs from aligned PCPs.
19. Risk taking PCPs can be terrific customers for value-based solutions (including payer-owned ones), provide them with fair economics, higher engagement, and better data for targeting the right patients.
But the bar for evidence will be high
But the bar for evidence will be high
https://twitter.com/Farzad_MD/status/1448662506512150546?s=20
• • •
Missing some Tweet in this thread? You can try to
force a refresh