1/93 Dismantling health resources and infrastructure is not a solution to the pandemic
OzSAGE calls for strengthened Public Health Measures and coordinated COVID-19 care in the community
30th December 2021
OzSAGE calls for strengthened Public Health Measures and coordinated COVID-19 care in the community
30th December 2021
2/93 Background -
OzSAGE is deeply concerned about COVID-19 in NSW, which is already affecting all of Australia. We commend the NSW government for reinstating mask mandates and QR code check ins. The decision to remove restrictions just as Omicron surged has cost us dearly.
OzSAGE is deeply concerned about COVID-19 in NSW, which is already affecting all of Australia. We commend the NSW government for reinstating mask mandates and QR code check ins. The decision to remove restrictions just as Omicron surged has cost us dearly.
3/93 We now have over 11,000 cases a day in NSW, a testing system that cannot keep up with demand and a health system so burdened that citizens are being told they may not be able to access healthcare. All models to date assumed good testing capacity and adequate contact tracing.
4/93 Without these, case numbers will blow out further. At this point in time there is no publicly available modelling to support a National Plan that is based on public health advice and which will protect our hospital systems from collapse.
5/93 Testing disaster -
Testing in NSW has exceeded capacity, with many people turned away after waiting in queues for hours and many testing centres shut. Regional and remote areas have even less capacity. There are unacceptable delays in testing results being sent.
Testing in NSW has exceeded capacity, with many people turned away after waiting in queues for hours and many testing centres shut. Regional and remote areas have even less capacity. There are unacceptable delays in testing results being sent.
6/93 Further, there have been over a thousand infected people who were sent a negative test result by mistake, and this problem has not been addressed in a transparent fashion.
7/93 Rather than investing in expanded testing capacity, the response of government is to restrict access to testing by changing the definition of close contacts and allowing PCR test to only family contacts, health workers and a few other groups.
8/93 This will reduce our surveillance capacity for new variants and give falsely low case numbers. In addition, test positive rates are in excess of 13% in NSW compared to under 2% during the Delta wave – telling us we need more, not less testing.
9/93 People are now being urged to avoid testing centres and hospitals, and to do their own testing using Rapid Antigen Tests (RATs).
10/93 These cost $12 to $20 or more for a single use test and are unaffordable for low-income people and families, given the need to test multiple times during the pandemic. Currently, there is a severe shortage of RATs nationwide.
11/93 This means even where people can afford them and could help relieve the pressure on the laboratories, they simply cannot buy a RAT kit.
12/93 We commend the Victorian government’s announcement of procurement of RATs to distribute free of charge to Victorians, and the Federal government’s announcement that they will co-fund the provision of RATs with states.
13/93 RATs are useful for screening of asymptomatic cases, but cannot serve as the backbone of the public health test and control system.
14/93 The results are not reported to the government, so people who test themselves and self-manage their COVID-19 will not be counted in official case numbers.
15/93 There is unknown accuracy of individual RAT brands with the Omicron variant, as a nasal swab (the usual method) is less likely to be positive than a throat swab. There has been no messaging to advise people on swabbing both the nose and throat when doing a RAT.
16/93 There should still be a requirement for a PCR testing after a positive RAT.
17/93 We are disturbed by the repeated messaging that only symptomatic people should get tested, when 40-45% of transmissions are asymptomatic, and even in people who develop symptoms, the peak of infectiousness is in the 2 days before symptoms begin.
18/93 The false reassurance of the messaging will result in more cases of viral transmission that otherwise would have been prevented.
Who is a close contact? -
We have previously outlined the importance of contact tracing and QR codes.
Who is a close contact? -
We have previously outlined the importance of contact tracing and QR codes.
19/93 The proposed change to the definition of a close contact is to reduce testing and resources and is not based on sound public health principles. Close contact definitions need to be based on risk. Risk is related to the amount of exposure to virus-laden aerosols.
20/93 Risk is not limited to arbitrary 4-hour time frames within households. Settings like nightclubs and restaurants have been sites of superspreading events, and if people exposed in these settings cannot get a PCR test, spread will accelerate.
21/93 Case numbers matter – it's simple maths -
The rhetoric that case numbers ‘do not matter’ is incorrect - particularly in the face of the Omicron variant. Daily case numbers are now 10 times higher than during the Delta wave and may be 100 times higher in January.
The rhetoric that case numbers ‘do not matter’ is incorrect - particularly in the face of the Omicron variant. Daily case numbers are now 10 times higher than during the Delta wave and may be 100 times higher in January.
22/93 Even if hospitalisation rates are lower with Omicron compared to Delta, a halving of hospitalisation rates with a 10-fold or 100-fold increase in cases will still translate to a high burden on the health system.
23/93 This is likely to overwhelm the health system, with regional services at particular risk.
24/93 A basic queuing model of hospitalisations & ICU occupancy rates , fitted to NSW’s Delta outbreak of July-October 2021, indicates that hospitalisation and ICU occupancy rates are now smaller fractions of reported case numbers than they were during the Delta outbreak. 

25/93 However, the trajectory of observed data suggest that hospitalisation and ICU occupancy are on a steeply rising trend and anticipated to exceed earlier peaks quite soon. 

26/93 In other words, optimistic assumptions about the impact of the Omicron variant on hospital admissions are unrealistic.
27/93 Introducing a narrower close contact definition, when the test positivity rate is currently over 13% in NSW, is unlikely to improve the burden on the health care system and will instead fuel the outbreak.
28/93 Limiting the amount of testing reduces pressure on the test and trace system in the short term but will worsen the health system burden, because it will result in chains of transmission that could otherwise have been stopped.
29/93 Over the longer term these quick fix adjustments for resource reasons and better optics will be detrimental. about the impact of the Omicron variant on hospital admissions are unrealistic.
30/93 Introducing a narrower close contact definition when the test positivity rate is currently over 7% in NSW, is unlikely to improve the burden on the health care system and will instead fuel the outbreak.
31/93 Limiting the amount of testing reduces pressure on the test and trace system in the short term but will worsen the health system burden, because it will result in chains of transmission that could otherwise have been stopped.
32/93 Over the long term these quick fix adjustments for resource reasons and better optics will be detrimental.
33/93 Omicron less severe than Delta but similar to the 2020 virus -
The intrinsic virulence of the Omicron variant remains unknown, and is challenging to establish due to differences in population makeup, the effects of vaccination programs,
The intrinsic virulence of the Omicron variant remains unknown, and is challenging to establish due to differences in population makeup, the effects of vaccination programs,
34/93 and prior variant exposures across countries.
Preliminary data suggest that compared to the Delta variant, Omicron infections are 40-45% less likely to result in hospitalisation.
Preliminary data suggest that compared to the Delta variant, Omicron infections are 40-45% less likely to result in hospitalisation.
35/93 However, the Delta variant was significantly more virulent than the original strain of the virus, being at least twice as likely to lead to hospitalisation or death.
36/93 This means that the Omicron variant is at least as virulent as the original strain of SARS-CoV-2, with far greater vaccine escape, and cannot be described as mild. In the US, we are seeing rapid increases in hospitalisations in children.
37/93 As the virus moves into vulnerable populations and those at greater risk of severe disease such as older Australians, people with disability and Aboriginal and Torres Strait Islander people, we may see a rise in hospitalisation and death.
38/93 These consequences have already been observed in countries such as Denmark, which are a week or two ahead of Australia in the Omicron surge.
Chronic illness from COVID-19 -
We know nothing yet of the incidence of long COVID associated with the Omicron variant.
Chronic illness from COVID-19 -
We know nothing yet of the incidence of long COVID associated with the Omicron variant.
39/93 During the first wave in Sydney, one-third of people with mild-to-moderate COVID-19 were left with persistent symptoms, including shortness of breath and fatigue. Long COVID could impose an enormous economic and human cost on the Australian health system for years.
40/93 New research from the US shows the virus persists in the brain, the heart, the kidneys and many other organs long after the initial illness, so preventing disease now may prevent long term chronic illnesses.
41/93 We also know that in Australia and overseas, pandemic surges have prevented access to care for cancer diagnoses and treatments for heart disease, strokes and trauma. This has resulted in excess deaths for non-COVID illnesses.
42/93 Lack of access to healthcare and deaths at home -
Our health system, stretched before COVID-19, has had its capacity eroded by staff resignations and a blow-out in waiting lists.
Our health system, stretched before COVID-19, has had its capacity eroded by staff resignations and a blow-out in waiting lists.
43/93 The further impact on the health system, by the sheer number of Omicron cases, at this time of year especially, could be enormous.
44/93 The rapid rise in Omicron cases may mean we are only days away from seeing higher hospitalisation and ICU admissions than during the peak of Delta. Case numbers whether formally recorded or not, will continue to climb until an adequate Vaccine-Plus strategy is in place.
45/93 A person who has been hospitalised for COVID-19 is no longer counted in the hospital statistics once they have cleared the virus, even if they still require a high level of care.
46/93 Therefore, the true number of hospitalisations for COVID-19 related disease accruing in the wards and ICU is not transparent to the public. The number in Hospital for the Home or on the waiting list for that service is not transparent to public.
47/93 We also note that paediatric admissions to Hospital in the Home, wards and ICU are accruing. We note that the shortage of staff is such that they are now asked to work after shorter isolation and that there is concern for burn out and fatigue.
48/93 NSW recognises the overload of the hospital system and is already warning the community not to expect access to hospital care. One week ago, NSW Health advised people under 50 years to care for themselves at home, without access to Hospital in The Home.
49/93 This week, they have revised the age cut off to anyone under 65 years.
50/93 This is the ultimate in “personal responsibility” – where citizens are left without access to healthcare and to sort out their own COVID care, as well as do their own contact tracing whilst sick with COVID-19.
51/93 Consideration should be given to support for people found COVID-19 positive who are in caring roles.
The consequence of this policy is that people may die at home when their lives could have been saved by proper timely healthcare.
The consequence of this policy is that people may die at home when their lives could have been saved by proper timely healthcare.
52/93 Without the safety net of regular contact from medical services the unintended consequences are likely to be more ambulance callouts and emergency department presentations.
53/93 OzSAGE tracked reported deaths at home in NSW during the Delta wave and found that there were a disturbingly high number of deaths of relatively young people with COVID-19 at home between July and October 2021.
54/93 During the Delta wave, we calculated the mean age of people dying at home from COVID-19 to be around 40 years of age, with some in their 20s and 30s (based on public reports from NSW).
55/93 During any other time, this would have been a national scandal, but it passed without comment or scrutiny from policy makers and health authorities.
56/93 We remain deeply concerned that people with preventable and treatable complications of COVID-19 may die at home in NSW, without access to even the support of Hospital in The Home.
57/93 If there is a wave of bed block, forced palliation in the home and the lack of any mass population planning for this means people who could have survived with hospital care may die of COVID at home, without any palliative care support to ease suffering.
58/93 Many younger people may slip through the cracks and crash at home, in plain sight of the whole family, with the moral injuries associated for all concerned.
59/93 We understand that National Cabinet is reviewing worker isolation/quarantine times in order to address the apparent staff shortages across critical health, first responder and essential workforce.
60/93 A further reduction in worker isolation/quarantine times may worsen infection rates of essential workers which will result in further staff shortages in essential workforces.
61/93 GPs expected to step in for failing hospitals -
The health system crisis response has been to ask people with COVID to self-care at home and call their GP if worried (rather than coming to hospital), at a time when many GPs are on holidays or running skeleton services.
The health system crisis response has been to ask people with COVID to self-care at home and call their GP if worried (rather than coming to hospital), at a time when many GPs are on holidays or running skeleton services.
62/93 This enormous surge in demand for GP services has not been funded or supported. Much of the palliative care burden will also fall to GPs as the hospices will not have capacity to manage people dying of COVID-19.
63/93 GPs will also have to cope with the surge in demand for vaccination for 3rd dose boosters and children 5-11 years.
64/93 'Self-care in the home' patients should be supported through GP Medicare funding that recognises the unique complexity of service delivery and coordination required through adequate additional MBS items for GPs and nurses, including telehealth and telephone services.
65/93 Changes in recommendations for boosters won’t get them into arms
Two doses of vaccine provides minimal protection against Omicron and wanes rapidly against Delta.
Two doses of vaccine provides minimal protection against Omicron and wanes rapidly against Delta.
66/93 While the changes to ATAGI guidelines for bringing forward the timing of boosters from “a minimum of 3 months” after January 31st are welcome, the lack of urgency in delivering boosters will allow both Delta and Omicron to spread.
67/93 In Victoria, state-administered vaccines have fallen dramatically despite the need for urgent action.
68/93 During the holiday season, when people are travelling and mixing more, there is a need to ramp up the messaging and the delivery of boosters to control transmission of COVID-19.
A fatalistic approach will be fatal for some people.
A fatalistic approach will be fatal for some people.
69/93 The “let it rip” strategy and defeatist narrative that “we are all going to get it” ignores the stark lived reality of the vulnerable of our society.
70/93 Despite 3 doses of vaccine, some patients with cancer and other immunosuppressed people, have substantially reduced protection against Omicron.
71/93 Similarly, people with co-existing health conditions (estimated to be 50% of the adult population) are at increased risk of illness.
72/93 The impacts of a fragmented testing system and disrupted health system will be felt most by our elderly, lower socio-economic groups, First Nations people, people with disability and regional populations.
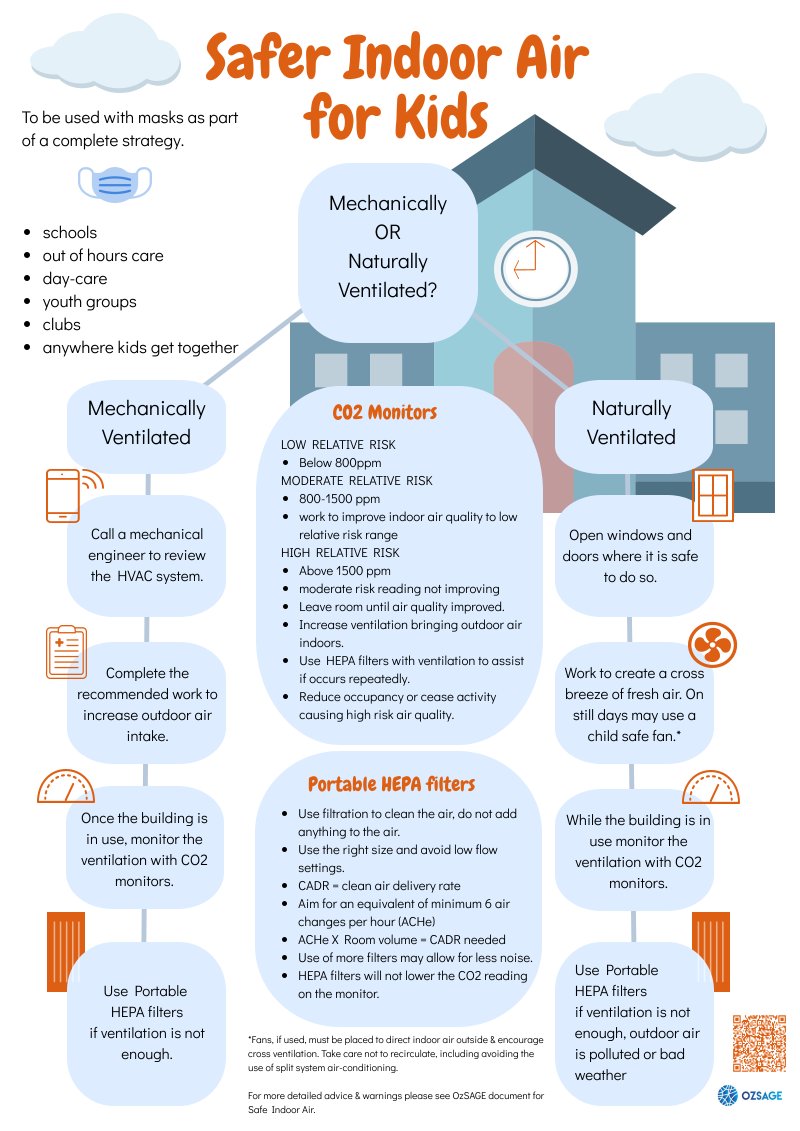
73/93 We must keep public health measures in place to protect these populations and ensure no-one is left behind. A fatalistic approach will be fatal for some people. OzSAGE is deeply concerned that children who are unvaccinated are completely unprotected.
74/93 Already a 10 year old has died in NSW. Children’s hospitalisations are increasing in both the UK and USA. The failure to make schools and childcare centres safe from aerosol transmission of COVID-19 must be immediately addressed as we have already outlined.
75/93 Recommendations: -
* NSW Health should immediately conduct a transparent and open investigation into why a private pathology provider issued falsely negative test results to infected people and provide a solution to prevent this happening again.
* NSW Health should immediately conduct a transparent and open investigation into why a private pathology provider issued falsely negative test results to infected people and provide a solution to prevent this happening again.
76/93 * Medical advice and current modelling that forms the basis of a state or national COVID-19 response should be publicly available.
77/93 * The Federal government should procure adequate RAT supplies for Australia and make them free or at least subsidise the cost for all Australians. A national notification system for positive RATs should be developed.
78/93 * Disseminate information to labs and community about the need for nose and throat swabs for detection of Omicron, as nasal swabbing alone is less accurate. Most RAT tests are for nasal swabbing.
79/93 * Governments should amend misleading messaging that tells asymptomatic people they do not need to test. Anyone who has been in close contact should test, regardless of symptoms or location of the contact.
80/93 * A fit-for-purpose model of Hospital in the Home and a palliative care plan should urgently be implemented in all states to ensure adequate healthcare for COVID-19 patients who cannot access hospital care.
81/93 Leaving infected people without guaranteed access to a pulse oximeter or even telephone advice is unacceptable.
* We recommend additional funding for the provision of pulse oximeters to all people self-caring at home.
* We recommend additional funding for the provision of pulse oximeters to all people self-caring at home.
82/93 * Procure oxygen supplies to deal with the Omicron surge immediately.
* Transparent reporting of infected people self-caring at home, hospital in the home, as well as waitlists should be routine along with hospital or ICU numbers.
* Transparent reporting of infected people self-caring at home, hospital in the home, as well as waitlists should be routine along with hospital or ICU numbers.
83/93 * Deaths at home should be monitored and reported weekly (with an age breakdown), as an indicator of failure of the health system.
84/93 * Support services to provide vaccines to those populations who are still yet to receive both first and second doses and boosters, particularly for Aboriginal and Torres Strait Islander people.
85/93 Escalate the delivery of booster doses at all facilities immediately as per our previous advice.
86/93 * Create new ‘COVID-19 GP Management at Home’ MBS item numbers (or amend eligibility for existing GP Management Plan MBS item numbers to temporarily include ‘self-care in the home’ patients with access to GPMP MBS item numbers) via telehealth to set up initial COVID-19…
87/93 …care plans in the home and for additional GP and Nurse telehealth MBS item numbers to adequately support the ongoing provision of primary care in the home where necessary.
88/93 * Immediately reinstate MBS telehealth item numbers and remove hotspot declaration requirements and existing patient in previous 12 months restrictions to allow for all patients to be able to access telehealth.
89/93 * Immediately review the vaccine ordering system for General Practices and remove fortnightly allocation limits to allow General Practices to order the amount of vaccines they can deliver.
90/93 The MBS Schedule should be adjusted to allow for delivery of vaccines by General Practices in other settings to increase vaccine delivery rate (for example on Community Ovals in drive-through vaccination clinics similar to influenza clinics in 2020).
91/93 * An additional one-off payment should be made to General Practices based on the number of vaccines delivered to cover additional costs such as PPE, additional vaccine infrastructure, staffing and information technology costs.
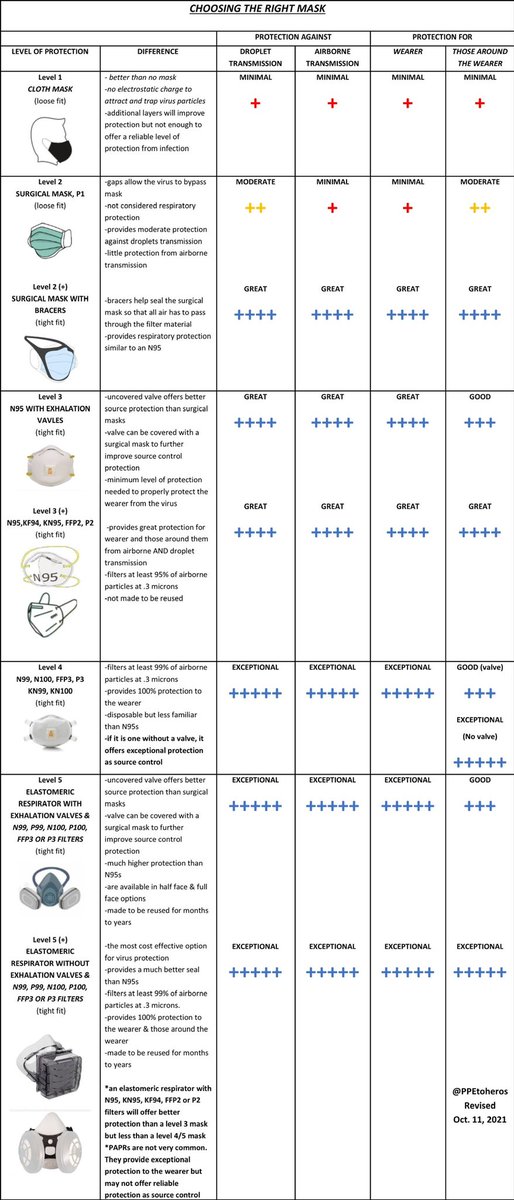
92/93 * If isolation/quarantine times are reduced we recommend that the reduction be no less than 7 to 10 days depending on the risk balance for the workforce/industry alongside a program of funded testing and respirator to reduce spread.
93/93 * Education to overturn the "we are all going to get it" messaging and enable the public and businesses to use simple prevention measures. This requires consistent national messaging on vaccines, masks and safe indoor air.
Full OzSAGE paper here: ozsage.org/wp-content/upl…
• • •
Missing some Tweet in this thread? You can try to
force a refresh