1/ Most hospitals will not be able to catch all healthcare worker infections, esp not before there is some nosocomial transmission to patients. These will largely start from the community & come into hospitals. Many levers to address here— universal N95 use during surges is one. 

2/ Why does this matter?
Bc hospitals have many patients who, despite vaccinations, are still at high risk of severe disease if they become infected
Patients should be able to feel safe & be safe in hospitals
The bare minimum we can do during surges is to wear N95 masks
Bc hospitals have many patients who, despite vaccinations, are still at high risk of severe disease if they become infected
Patients should be able to feel safe & be safe in hospitals
The bare minimum we can do during surges is to wear N95 masks
3/ We have likely under-counted in-hospital transmission of #covid19 — most hospitals are not tracking this to the level of detail that would confirm exactly where/ how transmission happened, & from whom and when for all cases
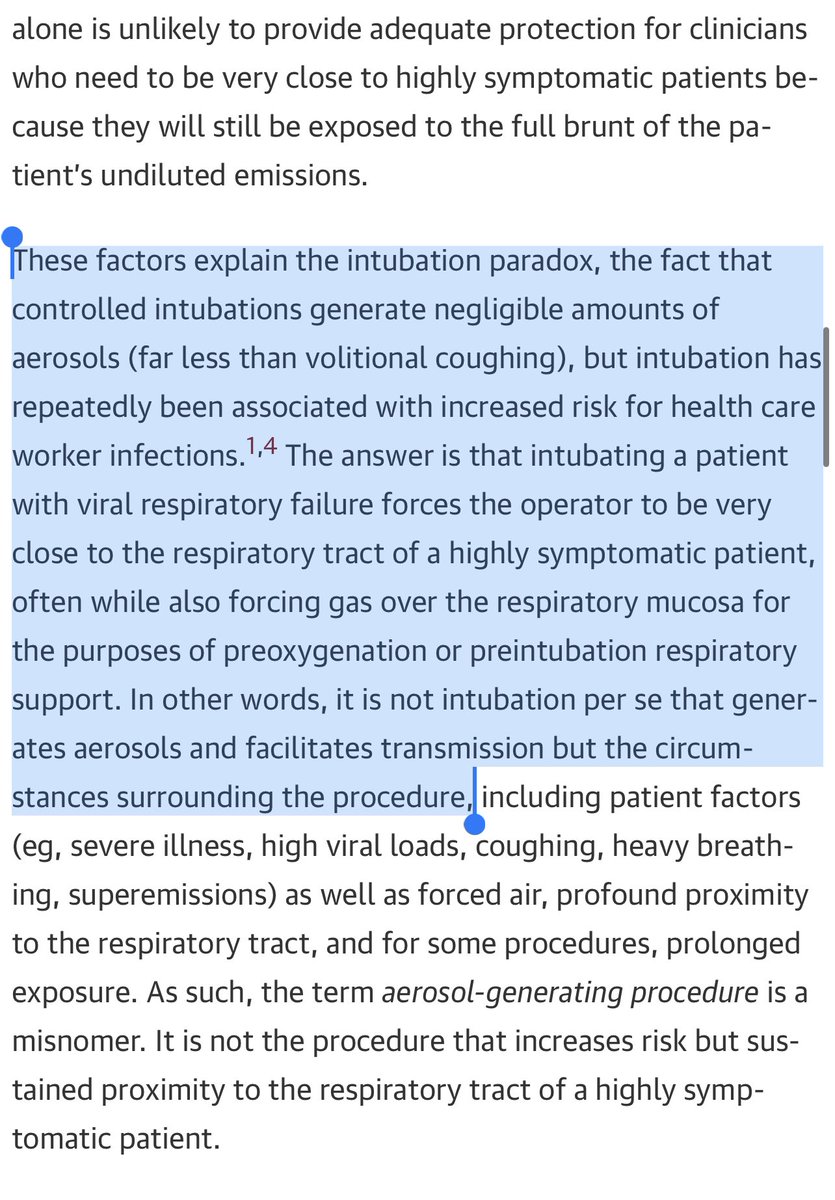
4/ High filtration fitted respirators provide much better source control than unfitted masks— meaning if I happened to be infected without knowing it, I would be exhaling very little that isn’t being filtered
Given most interactions with patients are very close up, this matters
Given most interactions with patients are very close up, this matters
5/ And all healthcare providers know that patient mask use in hospitals is often limited for many many reasons
So you don’t always get the added protection of two-way masking in these settings
Onus should be on the docs/nurses/staff in this case
So you don’t always get the added protection of two-way masking in these settings
Onus should be on the docs/nurses/staff in this case
6/ This can also protect healthcare workers as well!
It can reduce transmission between staff; it can also reduce occult transmission from patients to staff (some patients will test negative on screening but be early incubators; not all hospitals re-test for serial testing)
It can reduce transmission between staff; it can also reduce occult transmission from patients to staff (some patients will test negative on screening but be early incubators; not all hospitals re-test for serial testing)
Cc @choo_ek @meganranney @jeremyfaust @PaulSaxMD @MonicaGandhi9 @roby_bhatt @Bob_Wachter @drchethansathya @uche_blackstock @oni_blackstock @kj_seung @JoiaMukherjee @RanuDhillon @CarlosdelRio7 @V2019N @InfectiousDz
• • •
Missing some Tweet in this thread? You can try to
force a refresh