"A bag with feet."
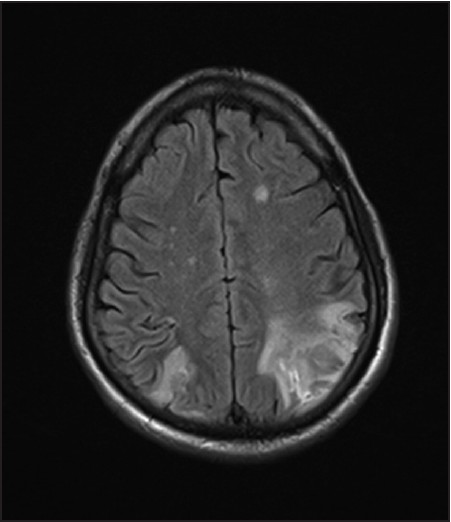
That's what the patient said he saw when we showed him the cookie jar picture. He was an older man who had been brought to the ED after being found driving his car around a field.
Here is what I think he was seeing:
#neurotwitter #tweetorial #MedEd
That's what the patient said he saw when we showed him the cookie jar picture. He was an older man who had been brought to the ED after being found driving his car around a field.
Here is what I think he was seeing:
#neurotwitter #tweetorial #MedEd

He was unable to focus on the whole picture at once.
This is a striking example of simultagnosia, which in his case was related to bilateral parieto-occipital strokes (Balint's syndrome.)
This is a striking example of simultagnosia, which in his case was related to bilateral parieto-occipital strokes (Balint's syndrome.)
Another way to test for Simultagnosia is to ask a patient what they see in a picture like this. They may only see T's and not the big H. 

Our patient also had the other classic features:
• Oculomotor apraxia (can't intentionally move his eyes towards an object.)
• Optic ataxia (can't accurately reach for something he was looking at.)
• Oculomotor apraxia (can't intentionally move his eyes towards an object.)
• Optic ataxia (can't accurately reach for something he was looking at.)
I get those terms confused sometimes, but it helps to focus on which part of the body isn't moving normally:
• OCULOMOTOR apraxia pertains to eye movements.
• Optic ATAXIA is the one that pertains to limb movements.
Here is ane example of optic ataxia:
• OCULOMOTOR apraxia pertains to eye movements.
• Optic ATAXIA is the one that pertains to limb movements.
Here is ane example of optic ataxia:
And finally, a musical non-sequitur.
Here is the song I haven't been able to stop humming while writing this thread. It is by the Adam Schlesinger, one of the great American pop songwriters, who died in April 2020 from COVID19 at the age of 52.
Here is the song I haven't been able to stop humming while writing this thread. It is by the Adam Schlesinger, one of the great American pop songwriters, who died in April 2020 from COVID19 at the age of 52.
• • •
Missing some Tweet in this thread? You can try to
force a refresh