Despite the dramatic title, Mr Snowdon raises an important point: what happens when number-crunchers neglect human factors.
I fear though, Mr Snowdon has succumbed to the very criticism he levy’s against those arguing for stronger mitigations
Thread
I fear though, Mr Snowdon has succumbed to the very criticism he levy’s against those arguing for stronger mitigations
Thread
https://twitter.com/cjsnowdon/status/1484834696152469507
This is not a criticism of the many astute and invaluable statisticians. More a challenge to basic assumptions.
Indeed, often the distance and objectivity is appreciated.
Indeed, often the distance and objectivity is appreciated.
https://twitter.com/cjsnowdon/status/1484864154305503238
But It is a pattern that seems to be emerging from economists and statisticians, that somehow the resistance of the PM to further mitigations was in some way a success.
While the economic argument seems absent, focus on healthcare numbers seems popular and problematic.
While the economic argument seems absent, focus on healthcare numbers seems popular and problematic.
The logic seems to be based either in the lack of understanding of what happens when healthcare capacity is compromised (the “well the NHS isn’t full” innocence). Or the focus on numbers (as is their job) versus the less tangible human consequences of such numbers.
Firstly, NHS capacity. Actually, just healthcare capacity.
Limits for safety are set at 85% bed occupancy (most of Europe use 80%).
The reason for this is the human factor…in this instance, the doctors, paramedics and nurses (and the public to some degree).
Limits for safety are set at 85% bed occupancy (most of Europe use 80%).
The reason for this is the human factor…in this instance, the doctors, paramedics and nurses (and the public to some degree).
As “beds” become limited we must make more risky decisions. A person we might have admitted at 80% capacity, we might not at 90% capacity.
We, as we have always done, adjust our admission criteria based on the demands on the service. This of course leads to sub-optimal care…
We, as we have always done, adjust our admission criteria based on the demands on the service. This of course leads to sub-optimal care…
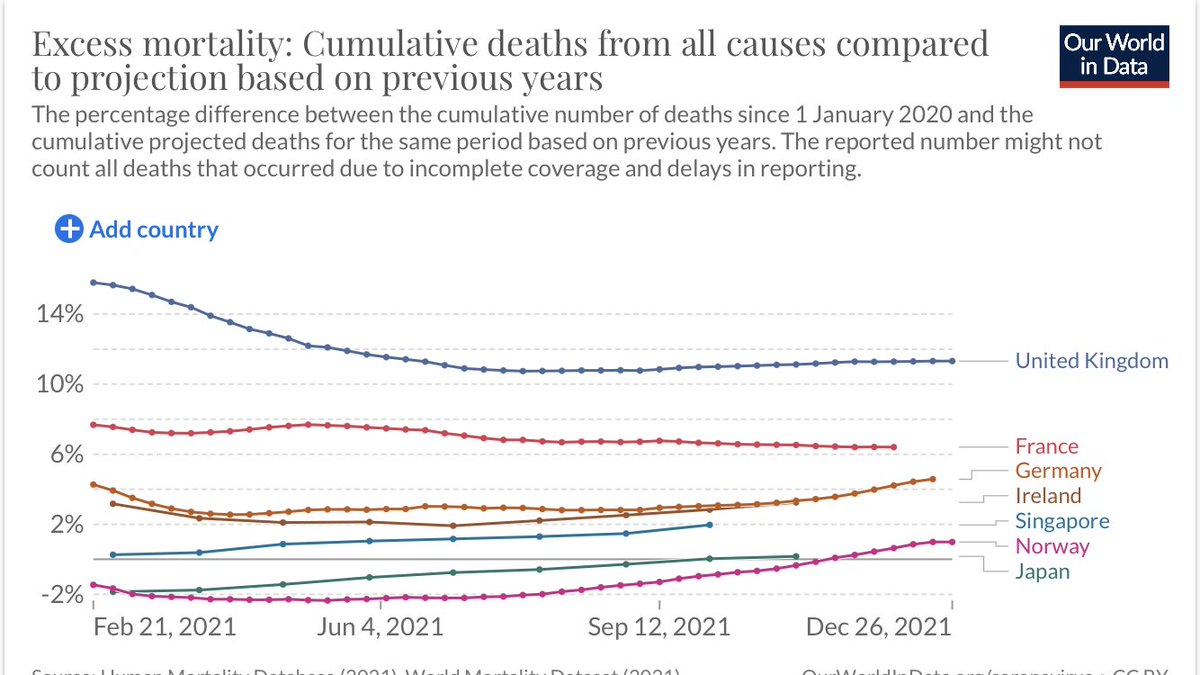
And when demands far outstrip availability (last 6 months), this leads to an increased mortality.
[1/3 not Covid]
[1/3 not Covid]

Also, Crucially, there is much higher morbidity or disability when care is sub-optimal. Delays in stroke or heart attack treatment leads to more brain or heart damage, for example.
https://twitter.com/seahorse4000/status/1484110260373794821
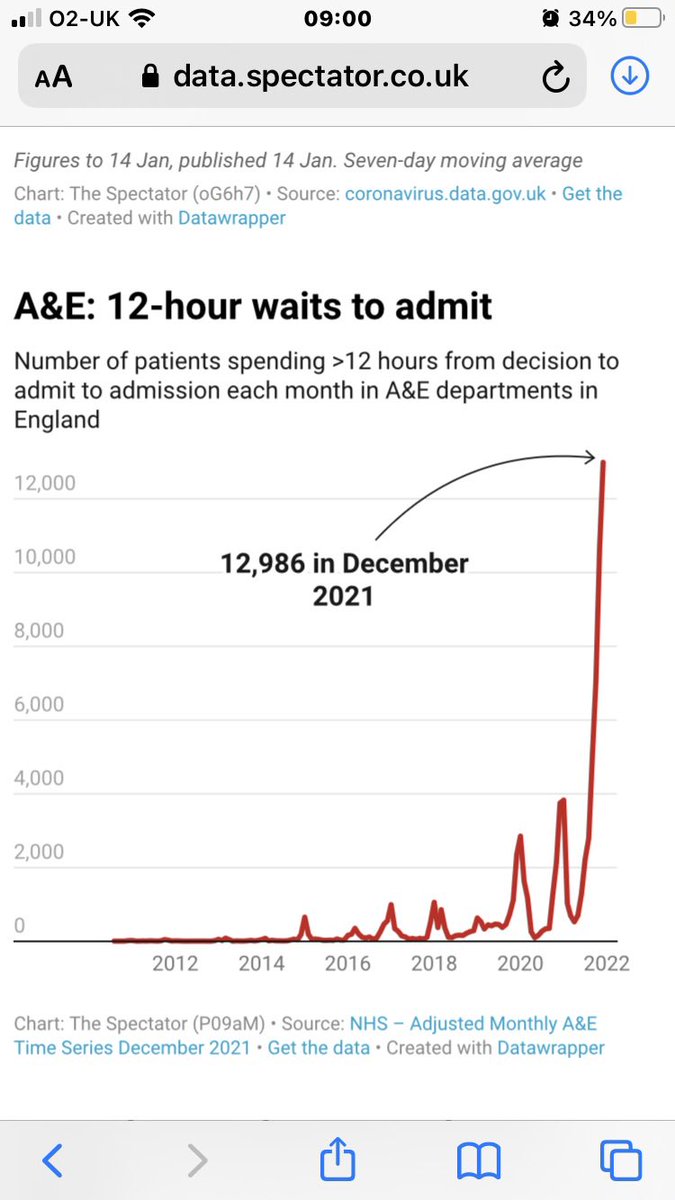
Post-freedom day (July) Delta surged to around 6% of total medical beds. You will note (above graph) excess deaths went from normal to above 10% also. Only 70% of these were Covid. 

But, note the effect on bed occupancy. 6% doesn’t sound like much, but 6% of the total, when there are only 15% available beds is around 40% of available capacity.
Combined with hospital capacity having been reduced since the pandemic started (a policy only current leadership could reconcile), we were already 4% down on available beds.
Combined, 2/3rds of our usually winter “contingency” was taken up by or due to Covid.
Combined, 2/3rds of our usually winter “contingency” was taken up by or due to Covid.
We started November with a bed occupancy of 94%. To my knowledge this has never happened prior to winter - more than 84% usually causes uproar (nhsproviders.org/nhs-winter-wat…)
Already, care was compromised even before Omicron took up 15% bed occupancy.
Already, care was compromised even before Omicron took up 15% bed occupancy.
But the true extent of the healthcare rationing needed to manage Omicron following the decision not to suppress, is difficult to quantify. It will though be felt and carried forward by the public and one can only imagine how such a historic event will play out on Election Day.
https://twitter.com/helengoldrick/status/1478822640995520512
Rationing healthcare should not be an acceptable strategy for managing waves of Covid infections. Certainly not in a high-income country. And the fact it continues two years on is an indictment of the bias/naivety applied to the data and the desperation for it to be over.
Whether it be this pandemic and a new variant or an entirely new pandemic, we will face this exact scenario once again. And if the infection fatality is even 1% higher, the choice for, as Chris says, society “hunkering down” may not be a political one. Life and livelihood at risk
Only the most stubborn amongst us would see investing in protections against pandemics as anything but the only logic prevailing from our experiences to date. Ventilation, quality mask availability, a functioning contact and trace, and a healthcare capacity fit for modern life.
Yes, we can argue it from an economic perspective. Healthcare capacity has been the reason for lockdowns…increasing our tolerance to pandemics would require investment in the frontline, for example.
But actually, the huge human cost and experience should be enough.
But actually, the huge human cost and experience should be enough.
So, using bed occupancy as never reaching 100% as any form of proxy for success is naive. The PMs decision not to do more was a monumental failure.
Flattening the wave may not prevent the infections over time, but it saves many lives and much disability.
Flattening the wave may not prevent the infections over time, but it saves many lives and much disability.
• • •
Missing some Tweet in this thread? You can try to
force a refresh