*NEW* Our latest study @AnnFamMed @RickGlazier1 shows that team-based primary care, coupled with payment reform, can improve patient outcomes & reduce ED use
annfammed.org/content/20/1/24
We desperately need to expand team-based primary care in Canada
(a mega 🧵)
annfammed.org/content/20/1/24
We desperately need to expand team-based primary care in Canada
(a mega 🧵)

#Primarycare is the foundation of a high-performing health system. Yet, primary care has been in crisis for the last 2 decades—challenged by an outdated payment model, growing patient need, rapidly growing evidence, and dysfunctional electronic medical record systems
Sharing the care with an interprofessional team has been seen for some time as an antidote to this crisis
Pharmacists, social workers, nurses and others can provide additional expertise and support to patients, particularly those with chronic mental and physical health issues
Pharmacists, social workers, nurses and others can provide additional expertise and support to patients, particularly those with chronic mental and physical health issues
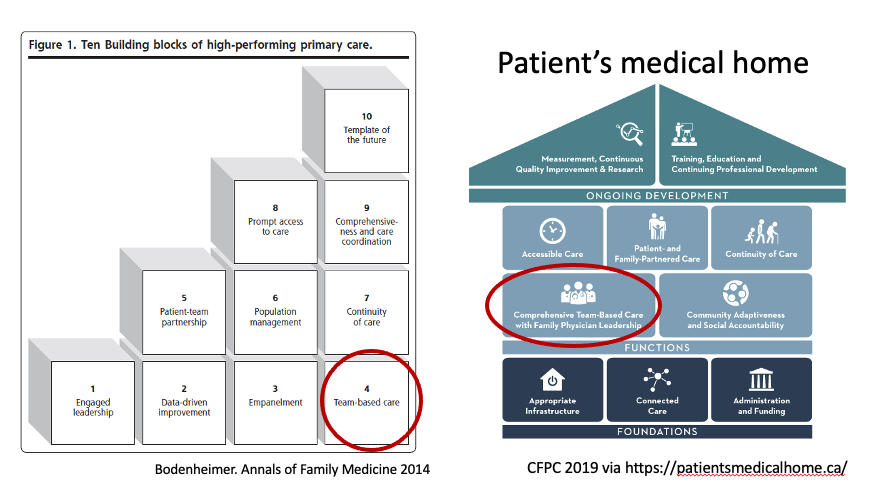
It's not surprising that interprofessional teams are seen as one of the 10 building blocks of high-performing primary care annfammed.org/content/12/2/1…
and a key pillar of a patient's medical home @FamPhysCan patientsmedicalhome.ca
and a key pillar of a patient's medical home @FamPhysCan patientsmedicalhome.ca
Many jurisdictions have introduced team-based care in some form but few to none have scaled these for the full population
Why? Many policy makers seem worried about return on investment
That's where our research comes in
Why? Many policy makers seem worried about return on investment
That's where our research comes in
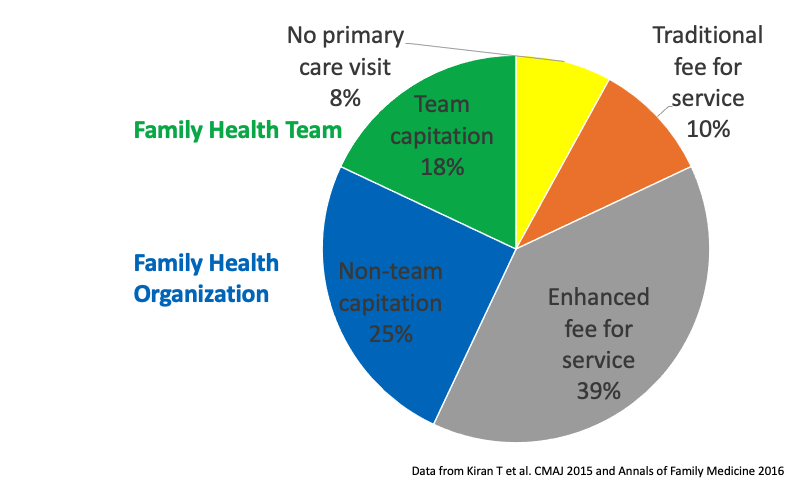
In Ontario, Community Health Centres have offered team-based care for decades but clinically serve <1% of the population
In 2005, Ontario introduced Family Health Teams, a new model of team-based care (and the one we studied)
In 2005, Ontario introduced Family Health Teams, a new model of team-based care (and the one we studied)
Doctors could apply to become part of Family Health Teams if they were already in one of Ontario's enrolment models where MDs were paid by capitation (that means instead of getting paid by the visit, they were paid a set fee per patient per year based on patient age and sex)
As part of a Family Health Team, the government would provide funding for other professionals to work alongside doctors. These could be nurses, nurse practitioners, social workers, pharmacists, dietitians and others
By 2011, ~20% of Ontarians received care as part of a Family Health Team (that number hasn't changed much) 
Family Health Teams were popular among doctors and their patients. But did they improve health outcomes or related costs?
Our current study looks to see what the impact of Family Health Teams were on patients using the emergency department (ED)
Our current study looks to see what the impact of Family Health Teams were on patients using the emergency department (ED)
Our study compared patients of MDs who transitioned to a Family Health Team (FHT) with patients of doctors who transitioned to a similar model (the Family Health Organization, FHO). In both cases, payment was by capitation but the FHT included access to an interprofessional team
We included data for 2,524,124 Ontarians and included outcome data (ie data on ED visit rate) from 2003 to 2017.
Patients' physicians transitioned to one of the new models sometime between 2006 and 2013 with most doing so before 2010
Patients' physicians transitioned to one of the new models sometime between 2006 and 2013 with most doing so before 2010
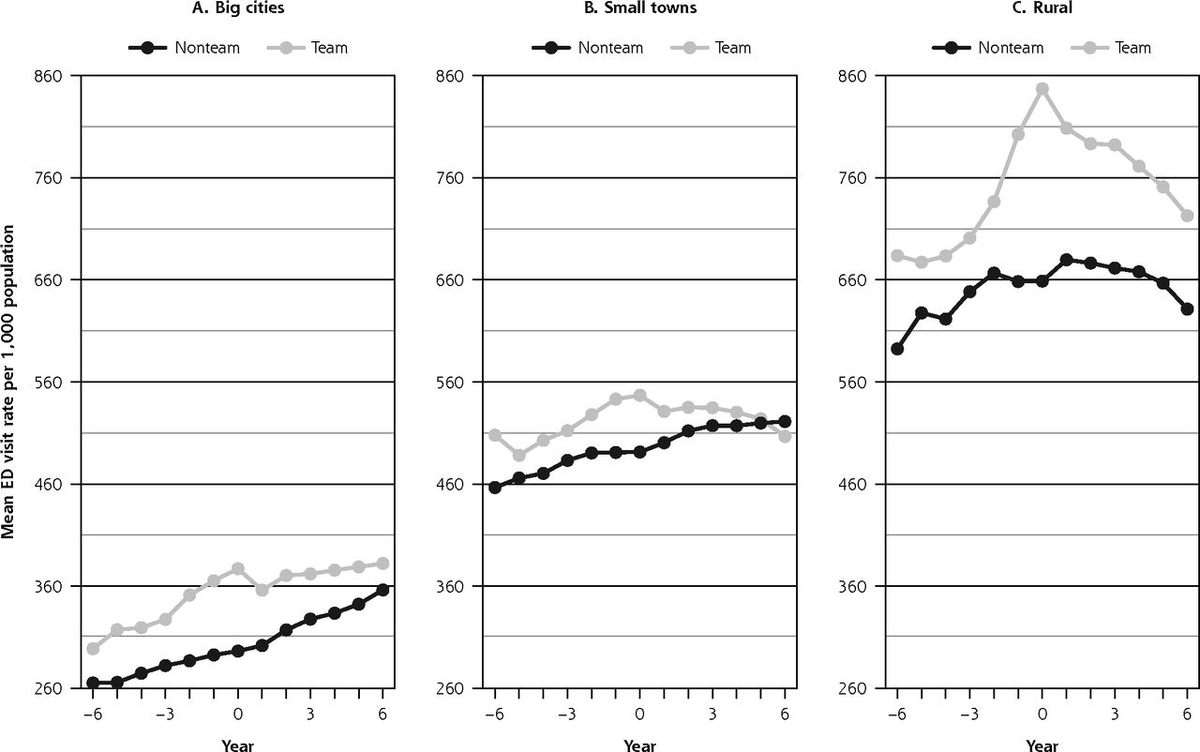
We looked to see how the ED visit rate changed for each group after transition to the new model. We looked separately at urban areas, small towns, and rural areas.
This graph shows the raw data with the year of transition set at zero. (FHT/team= grey, FHO/non-team = black)
This graph shows the raw data with the year of transition set at zero. (FHT/team= grey, FHO/non-team = black)
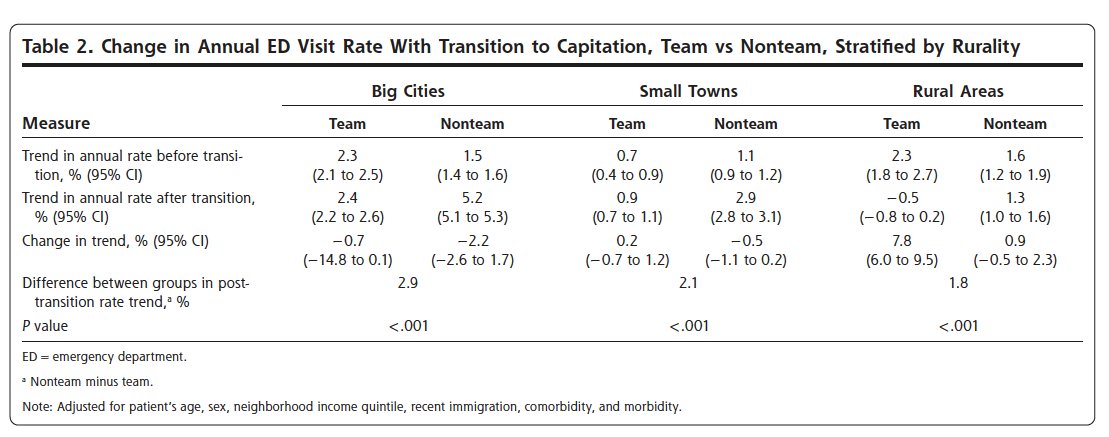
We then adjusted the ED rate by age, sex, income quintile and other patient factors so that we could try and isolate the affect of the transition to FHT/FHO
Here is that same graph showing the adjusted data
Here is that same graph showing the adjusted data
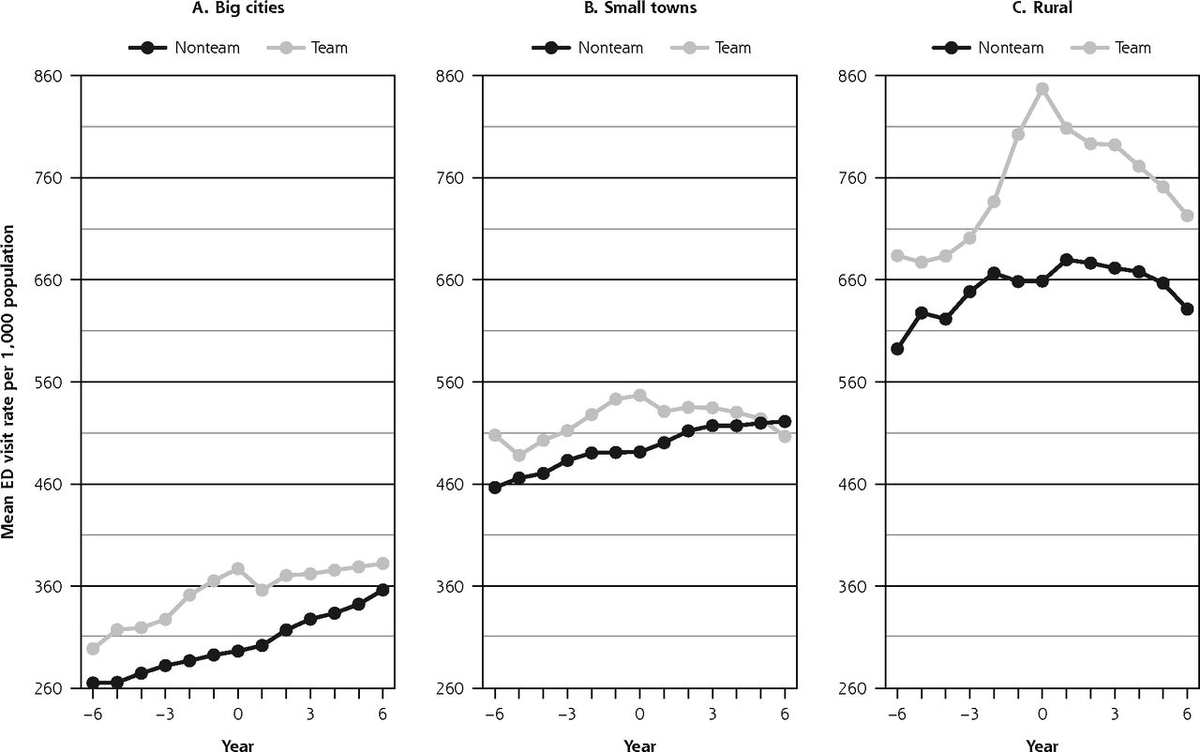
The graphs show that, in both groups, ED visits increased over time.
Patients in FHTs had higher ED visit rates before transition. But this increase in ED visits seems to have been blunted when they transitioned to the FHT
Patients in FHTs had higher ED visit rates before transition. But this increase in ED visits seems to have been blunted when they transitioned to the FHT
Our statistical calculations showed that, in big cities, the ED visit rate increased by 2.4% (95% CI, 2.2% to 2.6%) per year for the team group and 5.2% (95% CI, 5.1% to 5.3%) per year for the non-team group in the years after transition (P <.001) 
These findings held true even after we analyzed things using a different method (matching the FHO and FHT patients we were comparing based on their characteristics instead of adjusting for differences in characteristics using a regression model)
So what does this mean?
In short, we found that patients whose physicians joined a practice model combining capitation and team-based care had a slower increase in ED use compared with those whose physicians joined a capitation model without a team
In short, we found that patients whose physicians joined a practice model combining capitation and team-based care had a slower increase in ED use compared with those whose physicians joined a capitation model without a team
Our research can't tell you why but we have some hypotheses.
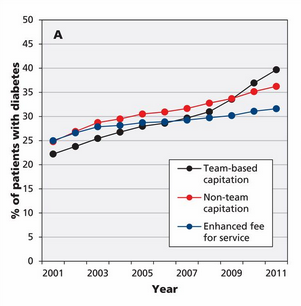
For one, the relative decrease in ED visits may relate to better chronic condition management. For example, people with better managed diabetes are less likely to need to go to hospital
For one, the relative decrease in ED visits may relate to better chronic condition management. For example, people with better managed diabetes are less likely to need to go to hospital
In fact, our previous work @CMAJ demonstrated that patients with diabetes who were part of Family Health Teams were more likely to see improvements in their diabetes care over time and more likely to get recommended testing
cmaj.ca/content/187/17…
cmaj.ca/content/187/17…
Another reason may relate to timely access. In particular, previous work we've done @CMAJ_Open has shown that patients of FHTs are more aware of their clinics after-hours clinics
cmajopen.ca/content/8/2/E3…
cmajopen.ca/content/8/2/E3…
It's an open question as to what team composition and roles are most likely to result in positive patient outcomes and decreased healthcare use
Tom Bodenheimer has written extensively on the topic including in this great @JAMAInternalMed pubmed.ncbi.nlm.nih.gov/30476958/
Tom Bodenheimer has written extensively on the topic including in this great @JAMAInternalMed pubmed.ncbi.nlm.nih.gov/30476958/
What our research—and the research of many others—makes clear is that team-based care adds value for patients and when done right, can reduce other types of health system use
But unfortunately the expansion of team-based care has stalled in Ontario
But unfortunately the expansion of team-based care has stalled in Ontario
There have been no new Family Health Teams in Ontario since 2012
@kellygrant1 wrote about this 7 years ago!
The government's decision was ostensibly related to concerns about cost and return on investment
I hope our research helps counter this concern
theglobeandmail.com/life/health-an…
@kellygrant1 wrote about this 7 years ago!
The government's decision was ostensibly related to concerns about cost and return on investment
I hope our research helps counter this concern
theglobeandmail.com/life/health-an…
Evidence is one input into the decision but values are another
Right now, our system in inherently unfair with some patients having free access to social work and other services while others don't
And sadly this distribution of resources is not rational
Right now, our system in inherently unfair with some patients having free access to social work and other services while others don't
And sadly this distribution of resources is not rational
In other research, @RickGlazier1 @ICESOntario has shown there is a 10-fold variation in availability of team-based care in regions across Ontario with no correspondence between availability and health care need 
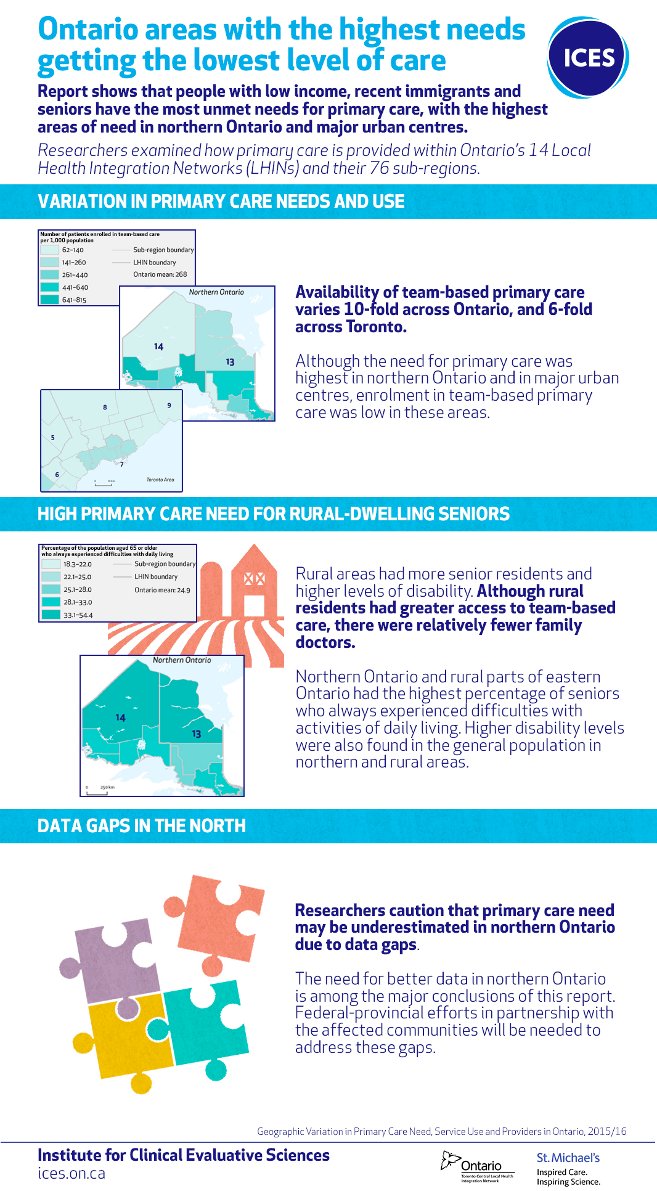
It's time to right this inequity and expand team-based care to all Ontarians—or at least ensure that resources are preferentially allocated to people with higher health-care need
As I've written about @HealthyDebate, I feel pretty lucky to practice in an amazing team healthydebate.ca/2015/10/about-…
Other doctors desperately want to practice in a team environment but there are no options open to them
Other doctors desperately want to practice in a team environment but there are no options open to them
I hope for a future where all Canadians have access to team-based care and all family doctors can choose to practice in a team model
There is a growing body of research that teams in primary care make sense for patients and physicians
It's also simply the fair way forward
There is a growing body of research that teams in primary care make sense for patients and physicians
It's also simply the fair way forward
Tagging a few colleagues who I suspect feel similarly
@RitikaGoelTO @DanyaalRaza @AndrewDPinto @AKLofters @NoahIvers @DrKateJMiller @KatharineSmart @nilikm @DocMCohen @NaheedD @AmitAryaMD @PhamTia @NadineLaraya @dpepe88 @DrJeffKwong @DrMichaelGreen1 @snewbery1 @AndreaChittle
@RitikaGoelTO @DanyaalRaza @AndrewDPinto @AKLofters @NoahIvers @DrKateJMiller @KatharineSmart @nilikm @DocMCohen @NaheedD @AmitAryaMD @PhamTia @NadineLaraya @dpepe88 @DrJeffKwong @DrMichaelGreen1 @snewbery1 @AndreaChittle
• • •
Missing some Tweet in this thread? You can try to
force a refresh