An in-depth review of Distal Humerus Fractures.
If you're interested in orthopedics you'll definitely want to check this review out.
1/12
If you're interested in orthopedics you'll definitely want to check this review out.
1/12

The distal humerus is composed of two columns, a medial and lateral column that are connected by the trochlea forming a triangular shape.
The distal humerus has:
40-45° anterior angulation
3-8° internal rotation
4-8° valgus
The distal humerus has:
40-45° anterior angulation
3-8° internal rotation
4-8° valgus

Distal humerus fractures most commonly occur in elderly females due to low energy falls, but may also occur in young adults due to MVA or sporting events.
On initial exam, it is important to do a careful neurovascular exam and assess the forearm compartments.
Avoid ROM testing due to the risk of neurovascular damage.
Undetected compartment syndrome may lead to a Volkmann ischemic contracture.
Avoid ROM testing due to the risk of neurovascular damage.
Undetected compartment syndrome may lead to a Volkmann ischemic contracture.

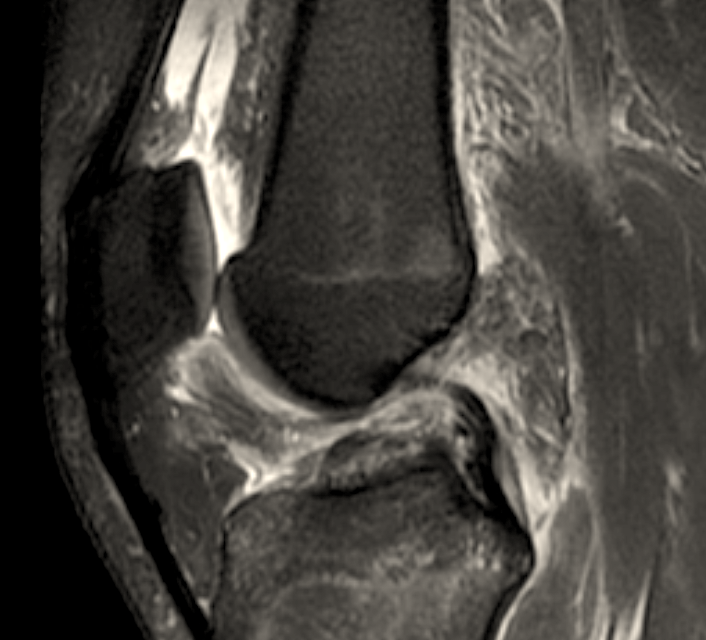
Obtain AP and lateral radiographs as well as a CT scan.
Traction films can reduce bony overlap and assist with surgical planning. (Shown on the right)
Traction films can reduce bony overlap and assist with surgical planning. (Shown on the right)

There are three main classification systems for distal humerus fractures:
AO/OTA
Milch: Unicolumnar
Jupiter: Bicolumnar
The remainder of this discussion will focus on bicolumnar distal humerus fractures.
AO/OTA
Milch: Unicolumnar
Jupiter: Bicolumnar
The remainder of this discussion will focus on bicolumnar distal humerus fractures.

Conservative treatment options include the bag of bones approach
A 2015 study by Aitken et al showed that at 46 months follow-up, 19 of 20 pts (of the original 40) had acquired functional ROM and the surgical intervention rate was determined to be <30% at 5 years post-injury
A 2015 study by Aitken et al showed that at 46 months follow-up, 19 of 20 pts (of the original 40) had acquired functional ROM and the surgical intervention rate was determined to be <30% at 5 years post-injury

Which of the following plating styles provides the strongest construct in distal humerus fractures?
Surgical options include:
Parallel plating (180°)
Perpendicular plating (90-90)
Total Elbow Arthroplasty
Biomechanical studies have shown similar strengths between parallel and perpendicular plating and plating choice depends on the fracture pattern and surgeon preference
Parallel plating (180°)
Perpendicular plating (90-90)
Total Elbow Arthroplasty
Biomechanical studies have shown similar strengths between parallel and perpendicular plating and plating choice depends on the fracture pattern and surgeon preference

Complications:
Most commonly elbow stiffness: though the majority of patients regain 75% of elbow motion.
--> the goal for functional ROM is 30-130°
Heterotopic ossification may occur in as many as 8%.
Hardware irritation, nonunion, and malunion may also occur.
Most commonly elbow stiffness: though the majority of patients regain 75% of elbow motion.
--> the goal for functional ROM is 30-130°
Heterotopic ossification may occur in as many as 8%.
Hardware irritation, nonunion, and malunion may also occur.
If you enjoyed this review please like or retweet to help the page grow and give us a follow!
Author: @CSMorford
#OrthoTwitter #MedEd #MedTwitter #DistalHumerus #Trauma #Orthopedics #Tweetorial #Radiology #Fractures #OrthoReviews
Author: @CSMorford
#OrthoTwitter #MedEd #MedTwitter #DistalHumerus #Trauma #Orthopedics #Tweetorial #Radiology #Fractures #OrthoReviews
• • •
Missing some Tweet in this thread? You can try to
force a refresh