
If COVID immunity can wane, what will happen after large epidemics peak? Some thoughts on post-epidemic 'honeymoon periods'... 1/
As immunity accumulates in a population (specifically immunity that protects against becoming infected/infectious), R will decrease. When R drops below 1, the epidemic peaks and starts to decline. But what might happen next? 2/
When R drops below 1, the epidemic doesn't magically end - it will continue to cause infections (and hence immunity) as it declines, meaning that the epidemic 'overshoots' the level of immunity required to get R below 1, potentially by quite a lot. 3/
So we can end up in a situation where R drops considerably below 1 as the epidemic continues to decline. End of story, right? Not quite... 4/
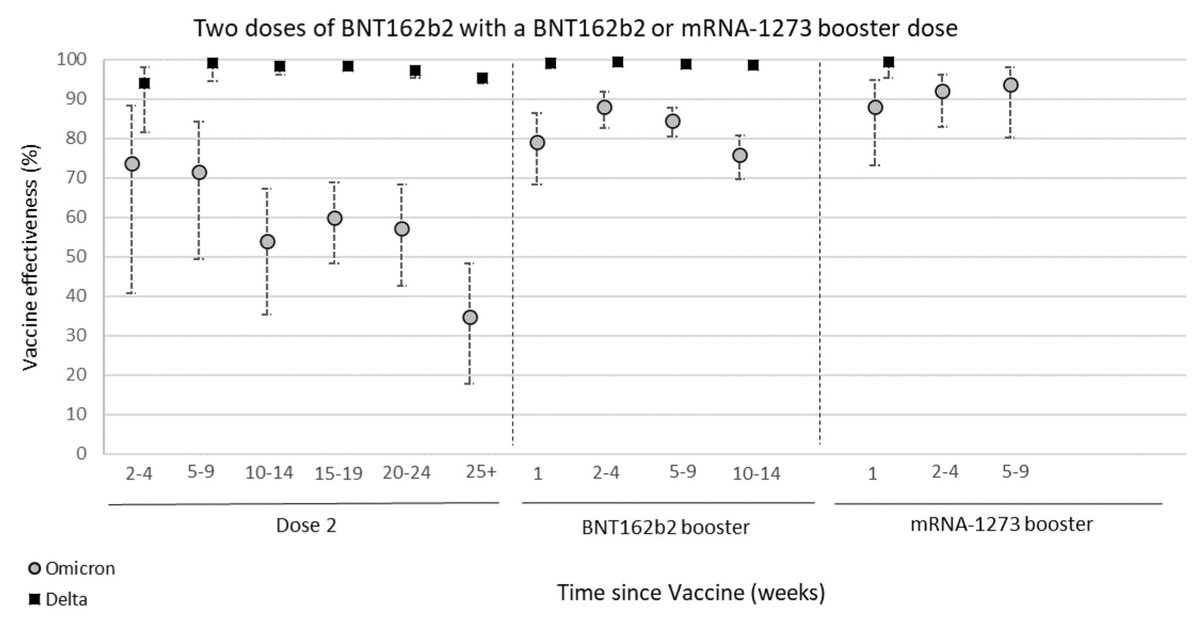
We know protection against infection can wane quickly for Omicron, e.g. below for immunity against symptomatic infection following vaccination (from: gov.uk/government/pub…) 5/ 

We also see evidence of some drop-off (although not as sharply) in protection against hospitalisation over time: 6/ 
But if R has dropped considerably below 1 during an epidemic, it will take some time for susceptibility to build up to sufficient levels to see a resurgence. Can therefore see a 'honeymoon period' where infection remains at lower levels for a while first. Here's a cartoon: 7/ 

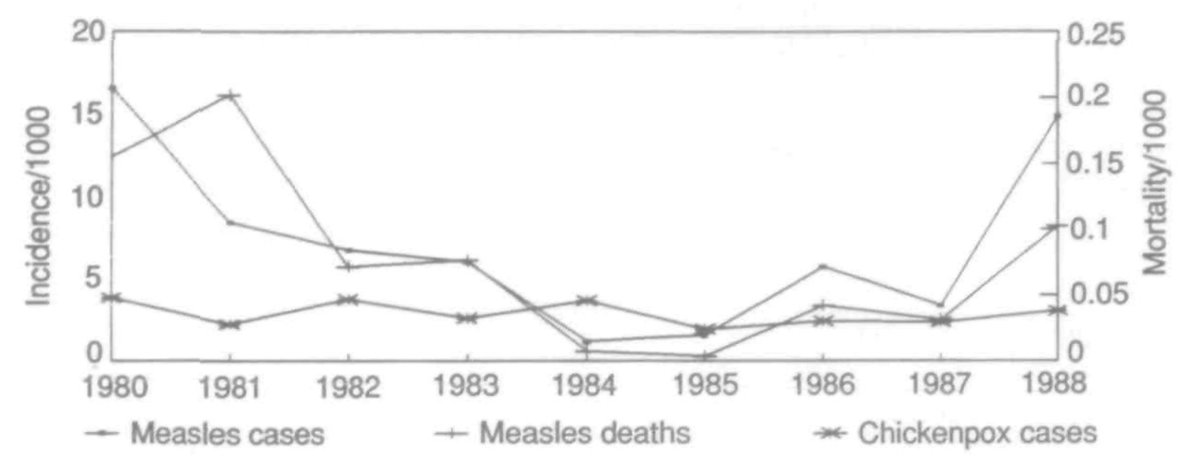
We can also see the honey period happen after the introduction of vaccination. The term 'honeymoon period' was first coined in the context of measles (ncbi.nlm.nih.gov/labs/pmc/artic…). In this case, new susceptibility arrives from new births rather than waning of existing responses. 8/
Below shows hypothetical dynamics after vaccination introduced with 50%, 75%, 80% coverage among infants after 4 years... 9/ 

Examples of a post-vaccination honeymoon period were later observed in countries ranging from BNurundi, below left (from: pubmed.ncbi.nlm.nih.gov/8194915/) to Mongolia, below right (from: pubmed.ncbi.nlm.nih.gov/17642531/). 10/ 


Several European countries may well have had a COVID post-vaccination honeymoon period against Alpha in early summer 2021, with vaccination + post-infection immunity driving down R. But we never saw subsequent effect of any waning, because Delta came along first. 11/
So in summary, we shouldn't assume that post-Omicron level of infection/disease is where things will stay for good. What's more, above only focuses on waning immunity (& new births in the case of measles), and new variants also likely to shape future susceptibility to COVID. 12/
• • •
Missing some Tweet in this thread? You can try to
force a refresh








