An in-depth review of Proximal Humerus Fractures.
If you're interested in orthopedics you won't want to miss this one!
🦴⚒️🧵👇
To view our past reviews visit: myorthoreviews.com
If you're interested in orthopedics you won't want to miss this one!
🦴⚒️🧵👇
To view our past reviews visit: myorthoreviews.com

Proximal humerus fractures are common, accounting for around 5% of all fractures with increasing frequency with age.
They are most common in elderly females and are considered a fragility fracture.
Which nerve is most commonly injured in proximal humerus fractures?
They are most common in elderly females and are considered a fragility fracture.
Which nerve is most commonly injured in proximal humerus fractures?
The axillary nerve passes medial to the surgical neck and is most commonly injured in proximal humerus fractures.
Sensation testing over the lateral shoulder may be performed as deltoid testing may be difficult.
Which artery provides the main blood supply to the humeral head?
Sensation testing over the lateral shoulder may be performed as deltoid testing may be difficult.
Which artery provides the main blood supply to the humeral head?
Previously the main blood supply was thought to be from the anterior humeral circumflex artery, but a 2010 study by Hettrich et al. published in @jbjs showed that 64% of the blood supply comes from the posterior humeral circumflex artery making it the main blood supply. 

A 2004 study by Hertel et al. described predictors of humeral head ischemia.
The two most critical factors were:
1) < 8 mm of calcar length
2) Medial Hinge Disruption
Increasing fracture complexity may also be associated with an increased risk of AVN.
The two most critical factors were:
1) < 8 mm of calcar length
2) Medial Hinge Disruption
Increasing fracture complexity may also be associated with an increased risk of AVN.

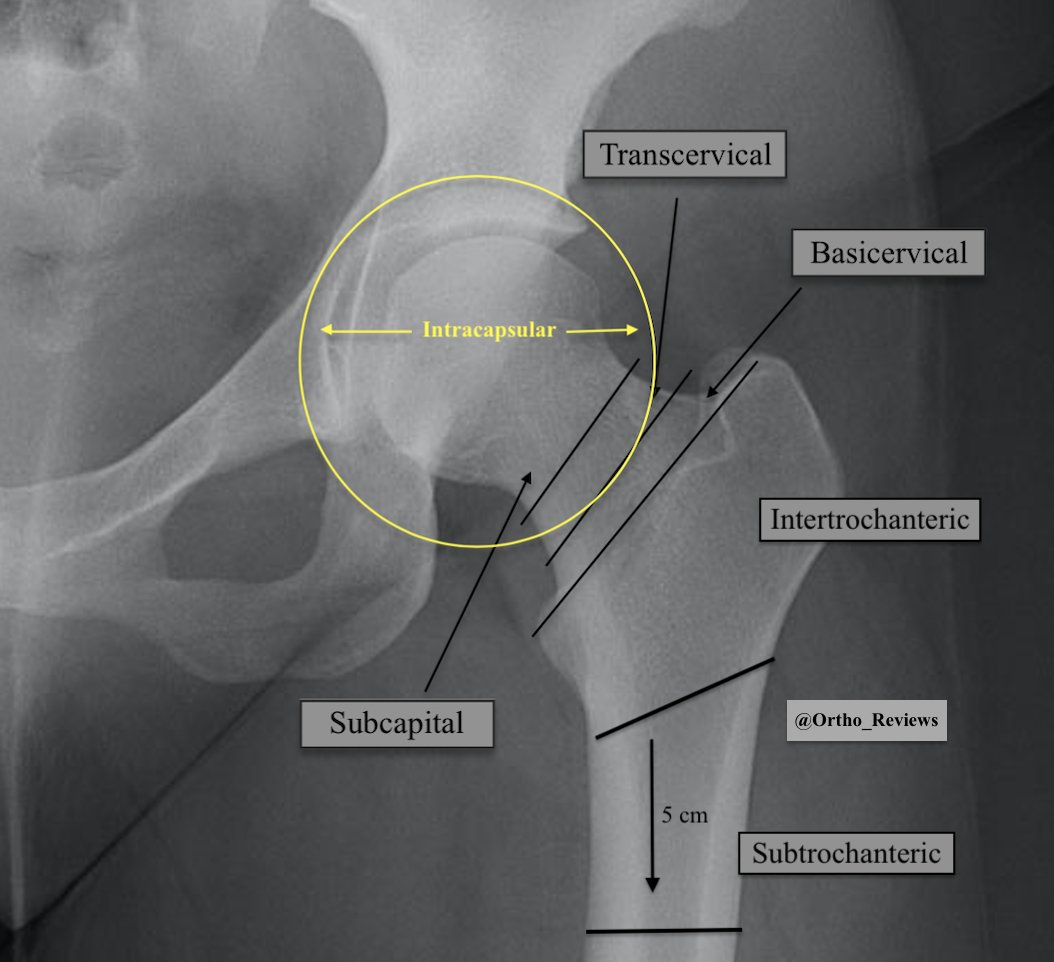
The proximal humerus has four bony segments:
✯ Humeral Head
✯ Greater Tuberosity (GT)
✯ Lesser Tuberosity (LT)
✯ Humeral Shaft
Fractures at the anatomic neck will produce a humeral head fragment and fractures at the surgical neck will produce a humeral shaft fragment.
✯ Humeral Head
✯ Greater Tuberosity (GT)
✯ Lesser Tuberosity (LT)
✯ Humeral Shaft
Fractures at the anatomic neck will produce a humeral head fragment and fractures at the surgical neck will produce a humeral shaft fragment.

Deforming forces on proximal humerus fragments:
✯ GT: Supraspinatus/Infraspinatus/Teres Minor
-Superior and ER
✯ LT: Subscapularis
-Medial
Surgical Neck Fractures:
✯ Proximal Fragment: Deltoid
-Abduction
✯ Humeral Shaft: Pec. Major
-Medial
✯ GT: Supraspinatus/Infraspinatus/Teres Minor
-Superior and ER
✯ LT: Subscapularis
-Medial
Surgical Neck Fractures:
✯ Proximal Fragment: Deltoid
-Abduction
✯ Humeral Shaft: Pec. Major
-Medial

The Neer Classification System for proximal humerus fx is based on the four bony segments.
A fragment is defined as having either:
✯ >10 mm displacement or
✯ >45° angulation
1-part fractures are ones without significant displacement, they may also be 2-part, 3-part, or 4-part
A fragment is defined as having either:
✯ >10 mm displacement or
✯ >45° angulation
1-part fractures are ones without significant displacement, they may also be 2-part, 3-part, or 4-part

Proximal humerus are forgiving and many can be treated non-operatively.
A 2015 study by Handoll et al. "The ProFHER Study" showed no difference in outcomes between non-operative and surgical management of surgical neck fx.
Of note: the mean age was 66 y.o. and 77% were female.
A 2015 study by Handoll et al. "The ProFHER Study" showed no difference in outcomes between non-operative and surgical management of surgical neck fx.
Of note: the mean age was 66 y.o. and 77% were female.
Most minimally displaced fractures can be treated with immobilization in a sling and swathe.
An axillary roll may be used to counteract the deforming force of pec. major in surgical neck fractures.
An axillary roll may be used to counteract the deforming force of pec. major in surgical neck fractures.
Operative indications are complex and vary by fracture pattern and age. Only general considerations will be discussed.
Which of the following has an operative indication of displacement > 5 mm, rather than >10 mm?
Which of the following has an operative indication of displacement > 5 mm, rather than >10 mm?
Greater tuberosity fractures with > 5 mm displacement may require surgical repair with ORIF due to their tendency to displace superiorly and cause impingement.
Options include cannulated screw fixation, tension band constructs, and suture anchoring.
Options include cannulated screw fixation, tension band constructs, and suture anchoring.

Displaced anatomic neck and head-splitting fractures are treated based on age.
Young patients:
✯ ORIF
Elderly patients:
✯ Anatomic vs. reverse shoulder replacement
RTS may be indicated if:
✯ low-demand patient
✯ deficient rotator cuff
✯ non-repairable tuberosities
Young patients:
✯ ORIF
Elderly patients:
✯ Anatomic vs. reverse shoulder replacement
RTS may be indicated if:
✯ low-demand patient
✯ deficient rotator cuff
✯ non-repairable tuberosities

Surgical management of 3-part fractures:
Young patients:
✯ ORIF with IM nailing or plate/screws.
Older patients:
✯ ORIF vs. shoulder replacement
Young patients:
✯ ORIF with IM nailing or plate/screws.
Older patients:
✯ ORIF vs. shoulder replacement

Complications:
✯ Humeral Head AVN following anatomic neck or head-splitting fractures treated with ORIF
✯ Non-union: most commonly varus deformity in surgical neck fx
✯ Hardware failure (combined cortical thickness > 4 mm has been suggested to be associated with reduced risk)
✯ Humeral Head AVN following anatomic neck or head-splitting fractures treated with ORIF
✯ Non-union: most commonly varus deformity in surgical neck fx
✯ Hardware failure (combined cortical thickness > 4 mm has been suggested to be associated with reduced risk)

If you enjoyed this review please retweet to help the page grow and give us a follow!
Author: @CSMorford
#ProximalHumerus #Fracture #Shoulder #Trauma #Ortho #Orthopedics #OrthoTwitter #Bones #Trauma #MedEd #MedicalEducation #MedTwitter #ERAS #Tweetorials #Radiology #OrthoReview
Author: @CSMorford
#ProximalHumerus #Fracture #Shoulder #Trauma #Ortho #Orthopedics #OrthoTwitter #Bones #Trauma #MedEd #MedicalEducation #MedTwitter #ERAS #Tweetorials #Radiology #OrthoReview
• • •
Missing some Tweet in this thread? You can try to
force a refresh