Tweet: renal sodium avidity in #HeartFailure
Do you ever wonder what is happening in the kidney in Heart Failure patients? Here’s a short #Tweetorial on renal physiology in HF (1/6).
#Cardiotwitter #Cardiology #FOAMed #Cardiorenal #MedEd #MedTwitter #Nephrology #ADVOR
Do you ever wonder what is happening in the kidney in Heart Failure patients? Here’s a short #Tweetorial on renal physiology in HF (1/6).
#Cardiotwitter #Cardiology #FOAMed #Cardiorenal #MedEd #MedTwitter #Nephrology #ADVOR
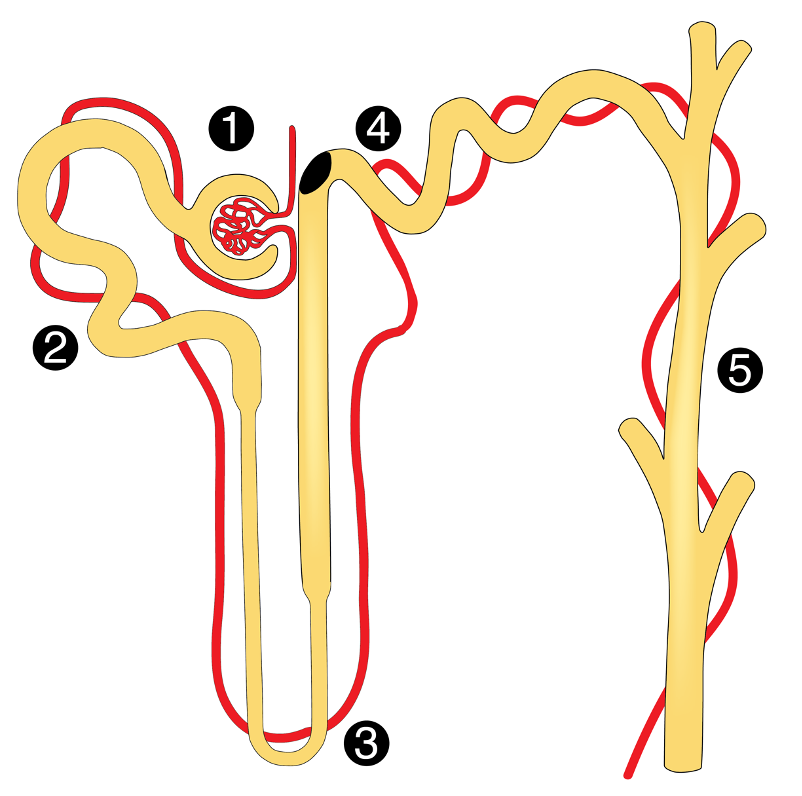
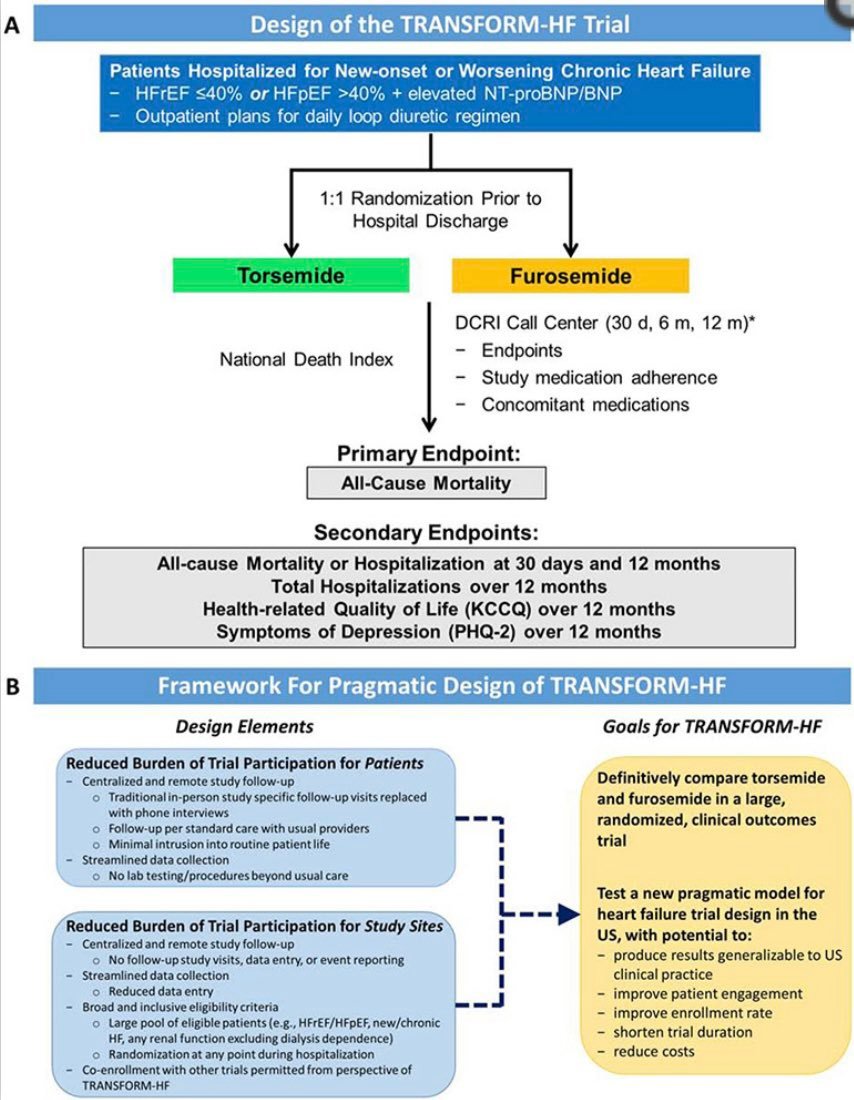
Glomerulus: renal blood flow ↓ in HF, but the kidney tries to maintain GFR by afferent arteriolar vasodilation and efferent arteriolar vasoconstriction. This leads to single-nephron hyperfiltration initially preserving total GFR, but further damaging the glomerulus. (2/6) 

Proximal tubules: hyperfiltration leads to ↑ water and solutes filtered, but ↓ remaining in the peritubular capillaries. Due to ↑ peritubular capillary oncotic pressure + ↑ renal lymph flow -> ↑ water and Na+ reabsorption in the proximal tubules (3/6) 
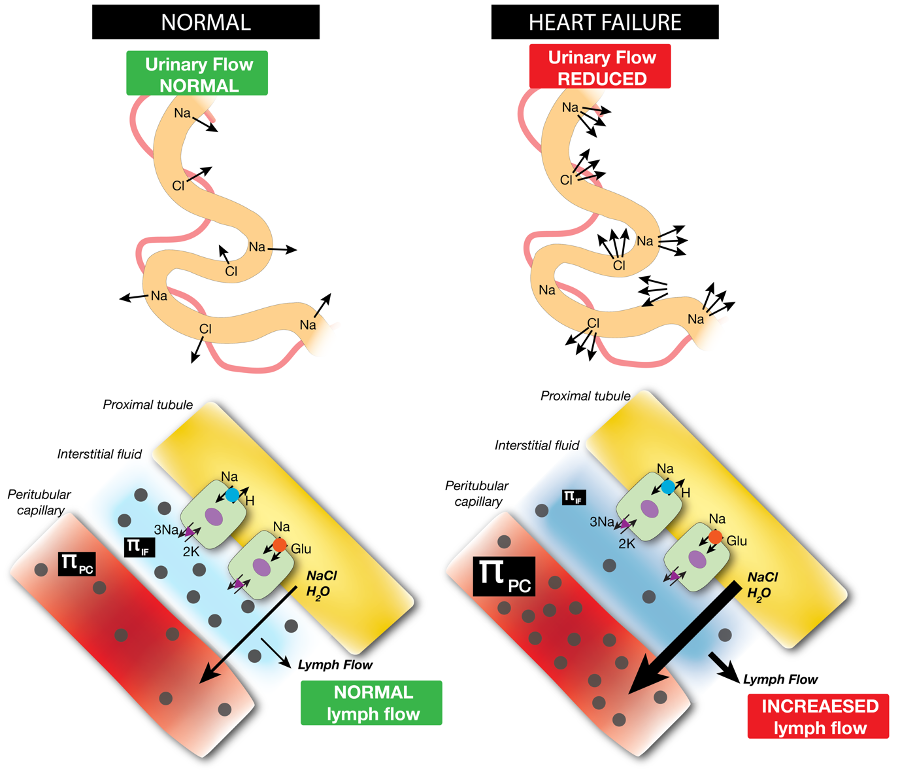
Henle: less fluid, Na+ and Cl- will reach the loop of Henle since more is proximally reabsorbed. Macula densa cells ↑ renin release due to ↓ Cl-. This ↑ glomerular hyperfiltration and RAAS/SNS activation (tubuloglomerular feedback) further promoting ↑ Na+ reabsorption (4/6) 

Distal parts: distal tubular flow is ↓ and aldosterone + ADH levels ↑, which ↑ remaining Na+ and water reabsorption (5/6) 

For an in depth review on the pathophysiology of renal sodium avidity in #HeartFailure doi: 10.1093/eurheartj/ehx035
@WilsonTangMD @FH_Verbrugge @petra_nijst @PieterMartensMD @JeroenDauw @kevin_damman @jozinetm
Tweetorial on GFR:
@WilsonTangMD @FH_Verbrugge @petra_nijst @PieterMartensMD @JeroenDauw @kevin_damman @jozinetm
Tweetorial on GFR:
https://twitter.com/FH_Verbrugge/status/1276990896660197376(6/6)

• • •
Missing some Tweet in this thread? You can try to
force a refresh