Summary tweet on my approach to anemias. credit to @n_gangat, @RichGodby, @zhuoerxie, Dr Ron Go, @VincentRK for teaching. Comments/critiques welcome!
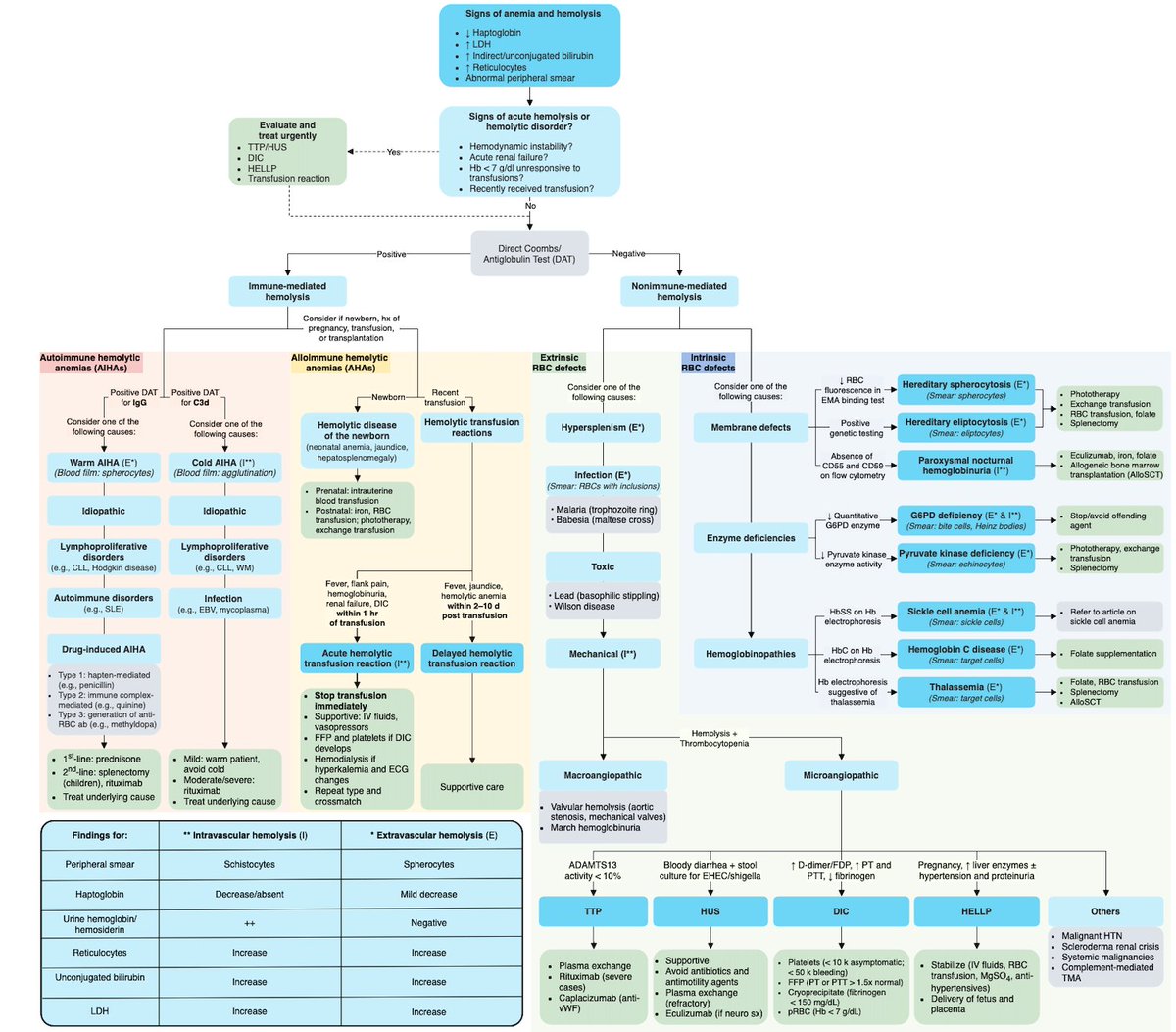
1. Approach to anemia
1. Approach to anemia

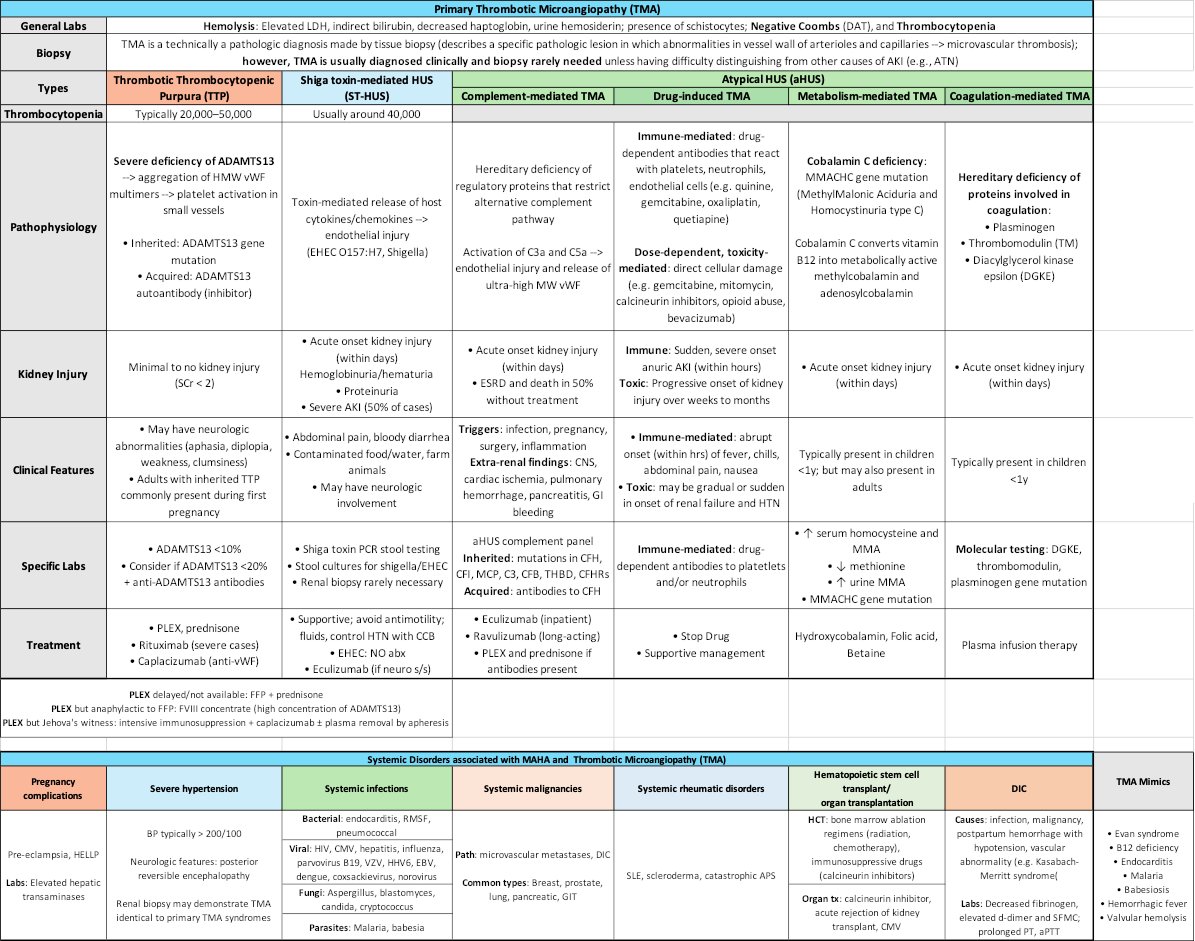
Another pearl. TTP suspected
- No PLEX? --> use FFP (contains ADAMTS13)
- FFP allergy? --> use FVIII concentrate (contains ADAMTS13)
- No PLEX? --> use FFP (contains ADAMTS13)
- FFP allergy? --> use FVIII concentrate (contains ADAMTS13)
• • •
Missing some Tweet in this thread? You can try to
force a refresh