ABG vs VBG:
- pH: VBG
- pCO2: VBG (not accurate in shock or hypercapnia); ABG for severe shock or if precise pCO2 needed in hypercapnia
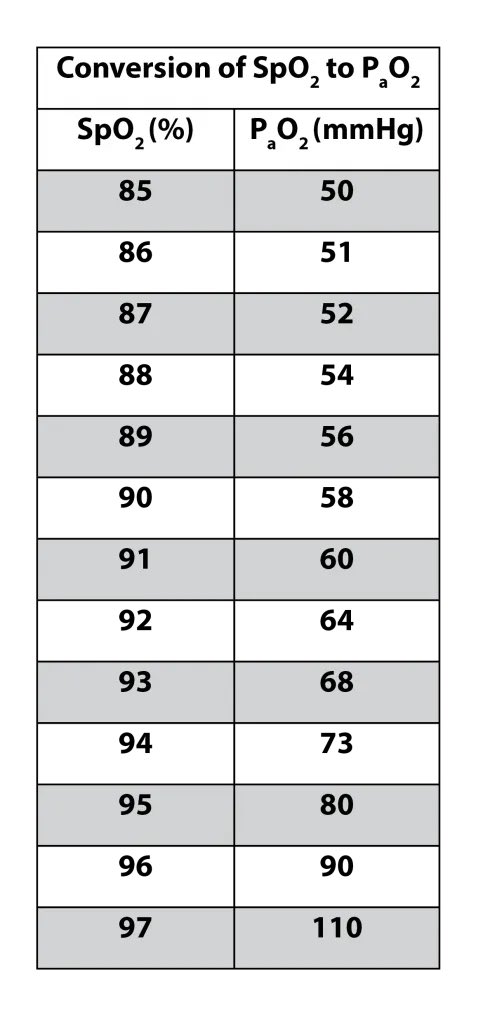
- PO2: ABG (but SpO2 generally good enough)
- CO or methemoglobin: co-ox
- pH: VBG
- pCO2: VBG (not accurate in shock or hypercapnia); ABG for severe shock or if precise pCO2 needed in hypercapnia
- PO2: ABG (but SpO2 generally good enough)
- CO or methemoglobin: co-ox
Causes of dissociation between SpO2 and PaO2
- shift in oxyHb curve
- dyshb: CO, methemoHb, sulHb
- Equipment failure
- Venous blood sample
- Localized hypoxemia (e.g., ischemic limb)
- Excessive oxygen consumption after sample collection (e.g., leukocytosis, thrombocytosis)
- shift in oxyHb curve
- dyshb: CO, methemoHb, sulHb
- Equipment failure
- Venous blood sample
- Localized hypoxemia (e.g., ischemic limb)
- Excessive oxygen consumption after sample collection (e.g., leukocytosis, thrombocytosis)

Saturation gaps: > 5% difference between SaO2 (ABG) and SpO2 (pulse ox)
- SaO2 (or PaO2) > SpO2: methemoglobin, sulfhemoglobin
- SpO2 > SaO2 (or PaO2): CO, cytosis, venous sample
journal.chestnet.org/article/S0012-…
- SaO2 (or PaO2) > SpO2: methemoglobin, sulfhemoglobin
- SpO2 > SaO2 (or PaO2): CO, cytosis, venous sample
journal.chestnet.org/article/S0012-…
• • •
Missing some Tweet in this thread? You can try to
force a refresh