
Another #CriticalCare #Tweetorial!
🫀Left Ventricular Assist Device for the non-cardiologist🫀
Join me on a journey through LVADs with some #FOAMcc highlights useful for #CritCare #EmergencyMedicine #HospitalMedicine #Meded
#EmoryNCCTweetorials
@CardioNerds @emoryheart
1/🧵
🫀Left Ventricular Assist Device for the non-cardiologist🫀
Join me on a journey through LVADs with some #FOAMcc highlights useful for #CritCare #EmergencyMedicine #HospitalMedicine #Meded
#EmoryNCCTweetorials
@CardioNerds @emoryheart
1/🧵

Goals for this #Tweetorial
1-Review the basics of what an LVAD is and does
2-Discuss indications for an LVAD
3-Review some common complications of the device itself
4-Review systemic complications of an LVAD
2/🧵
1-Review the basics of what an LVAD is and does
2-Discuss indications for an LVAD
3-Review some common complications of the device itself
4-Review systemic complications of an LVAD
2/🧵
Lets start with some basics of the LVAD. Historically the two most commonly encountered are the Heartmate 3 and the Heartware.
We will focus on the Heartmate 3 (Shown below)
3/🧵
We will focus on the Heartmate 3 (Shown below)
3/🧵
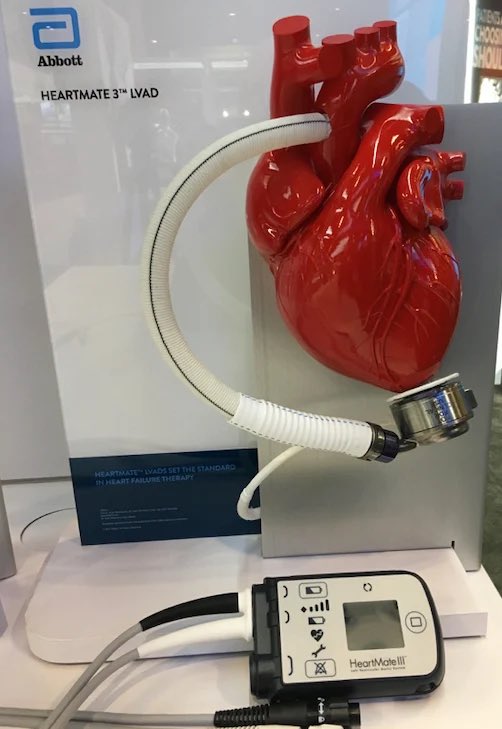
The Heartmate3 (HM3) is a centrifugal flow pump. It has a fully magnetically levitated motor and is bearingless, meaning the motor itself is contactless.
HM3 can pump 10L/min of blood directly from the LV to the ascending aorta.
4/🧵
HM3 can pump 10L/min of blood directly from the LV to the ascending aorta.
4/🧵

Outside the hospital your patient’s typical set-up will consist of battery packs on the shoulders, a driveline tunneled out of the abdomen, and the controller across a belt.
Each battery lasts 12-14hours. The controller has 15min of intrinsic backup battery as a safety.
5/🧵
Each battery lasts 12-14hours. The controller has 15min of intrinsic backup battery as a safety.
5/🧵

The HM3 motor can spin up to 5500x/min. This allows for near continuous flow, and in many patients will eliminate their pulsatility.
Meaning your patient might not have a pulse!
6/🧵
Meaning your patient might not have a pulse!
6/🧵
HOWEVER:
HM3 has a programmable setting which allows for deceleration/acceleration of the rotor by 2000rpm every 2seconds.
This allows for device washout and to eliminate stasis in the system, and can create pulsatility!
7/🧵
HM3 has a programmable setting which allows for deceleration/acceleration of the rotor by 2000rpm every 2seconds.
This allows for device washout and to eliminate stasis in the system, and can create pulsatility!
7/🧵
This great graphic from @rishikumarmd highlights the blood flow through the LVAD.
Its important to realize the LVAD doesn’t eliminate the intrinsic ability of the LV to pump blood across the aortic valve, just significantly reduces the work!
8/🧵
Its important to realize the LVAD doesn’t eliminate the intrinsic ability of the LV to pump blood across the aortic valve, just significantly reduces the work!
8/🧵

The LVAD includes a monitor
4 P’s of the LVAD:
Pump Speed: Programed in RPMs
Power: Amount of watts to create flow
Pump Flow: Basically CO, 4-6L/min typical
Pulse Index: Measure of native LV function. Lower Values mean less native LV function
9/🧵
4 P’s of the LVAD:
Pump Speed: Programed in RPMs
Power: Amount of watts to create flow
Pump Flow: Basically CO, 4-6L/min typical
Pulse Index: Measure of native LV function. Lower Values mean less native LV function
9/🧵

So who needs an LVAD?
Bridge-to-transplant: pt in need of support while awaiting donor organ
Destination Therapy: Pt with HFrEF and ineligible for heart transplant
Bridge-to-Decision: Pt with current (but reversible) CI to transplant
10/🧵
Bridge-to-transplant: pt in need of support while awaiting donor organ
Destination Therapy: Pt with HFrEF and ineligible for heart transplant
Bridge-to-Decision: Pt with current (but reversible) CI to transplant
10/🧵
More defined indications for LVAD:
-NYHA class IV for 60-90d
-Max Medical therapy
-Chronic dependence on inotropic agents
-LVEF<25%
-PCWP >/= 20mmHg
-SBP </= 80-90mmHg or CI < 2L/min/m2
11/🧵
-NYHA class IV for 60-90d
-Max Medical therapy
-Chronic dependence on inotropic agents
-LVEF<25%
-PCWP >/= 20mmHg
-SBP </= 80-90mmHg or CI < 2L/min/m2
11/🧵
So what complications do you need to watch out for?
Pump Thrombosis:
Turbulent flow-> thrombus formation in pump itself. More frequent w/1st and 2nd gen devices (up to 12.2%)
HM3 has a 1.1% pump thrombus rate at 2yrs. (@NEJM nejm.org/doi/full/10.10…)
12/🧵
Pump Thrombosis:
Turbulent flow-> thrombus formation in pump itself. More frequent w/1st and 2nd gen devices (up to 12.2%)
HM3 has a 1.1% pump thrombus rate at 2yrs. (@NEJM nejm.org/doi/full/10.10…)
12/🧵
As a 🧠 doc I am obviously concerned about neurologic complications!
Historically these occurred at a much higher rate, but still remains a primary cause of death at 6-24mo post-LVAD!
Based on MOMENTUM3 Trial of HM3 vs HM2 the risk of stroke is 10.1% w/HM3.
13/🧵
Historically these occurred at a much higher rate, but still remains a primary cause of death at 6-24mo post-LVAD!
Based on MOMENTUM3 Trial of HM3 vs HM2 the risk of stroke is 10.1% w/HM3.
13/🧵
Stroke in LVAD pts is about 50/50 ischemic and hemorrhagic.
Ischemic strokes can be due to embolic events or induced hypertension due to predisposition to uncontrolled HTN post-LVAD.
14/🧵
Ischemic strokes can be due to embolic events or induced hypertension due to predisposition to uncontrolled HTN post-LVAD.
14/🧵
Wait why do LVAD patients become hypertensive??
This has to do with ⬇️ pulsatility meaning the baroreceptors see ⬇️ pressure variation.
This ⬆️ sympathetic activation ⬆️ PVR and resulting in clinical HTN
See great review below in @StrokeAHA_ASA
ahajournals.org/doi/10.1161/ST…
15/🧵
This has to do with ⬇️ pulsatility meaning the baroreceptors see ⬇️ pressure variation.
This ⬆️ sympathetic activation ⬆️ PVR and resulting in clinical HTN
See great review below in @StrokeAHA_ASA
ahajournals.org/doi/10.1161/ST…
15/🧵
So how would you assess your LVAD patient’s BP if they don’t have a pulse!?!
Return to Flow (RTF)!
Measure using a manual BP cuff
Inflate to ~120mmHg
Slowly deflate w/doppler over brachial artery
Pressure reading where you get flow is your RTF and is equivalent to MAP!
16/🧵
Return to Flow (RTF)!
Measure using a manual BP cuff
Inflate to ~120mmHg
Slowly deflate w/doppler over brachial artery
Pressure reading where you get flow is your RTF and is equivalent to MAP!
16/🧵
The brain is great and all, but what about the other organs?
Other notable adverse events include right heart failure (due to increased left-sided output), GI bleeding, and driveline site infection.
nejm.org/doi/full/10.10…
17/🧵
Other notable adverse events include right heart failure (due to increased left-sided output), GI bleeding, and driveline site infection.
nejm.org/doi/full/10.10…
17/🧵

The most feared complication with an LVAD…
Cardiopulmonary Arrest!
This algorithm from AHA suggests an approach (made for prehospital)
CPR is OK but confirm LVAD is not working or not adequately perfusing!
In hospital- get your VAD team involved EARLY!
18/🧵
Cardiopulmonary Arrest!
This algorithm from AHA suggests an approach (made for prehospital)
CPR is OK but confirm LVAD is not working or not adequately perfusing!
In hospital- get your VAD team involved EARLY!
18/🧵

A brief comment on outcomes…
1yr survival w/HM3 is 86.6%, 2 yr is 79%.
Mean survival post-LVAD is 7.1 years (data pending on HM3). Compare this to a median survival post-heart transplant of 12yrs!
19/🧵
1yr survival w/HM3 is 86.6%, 2 yr is 79%.
Mean survival post-LVAD is 7.1 years (data pending on HM3). Compare this to a median survival post-heart transplant of 12yrs!
19/🧵
Thanks for joining to learn some basics of the LVAD!
Please comment with teaching points and corrections to mistakes!
@PatrickZakka @EmoryNeuroCrit @MedTweetorials @caseyalbin @JayKinariwala @AvrahamCooperMD @nickmmark @CardioNerds @neuro_intensive @criticalbeansmd
20/🧵
Please comment with teaching points and corrections to mistakes!
@PatrickZakka @EmoryNeuroCrit @MedTweetorials @caseyalbin @JayKinariwala @AvrahamCooperMD @nickmmark @CardioNerds @neuro_intensive @criticalbeansmd
20/🧵
References/Additional Resources:
1- nejm.org/doi/full/10.10…
2- @rishikumarmd Post on LVADs rk.md/2015/what-left…
3- ahajournals.org/doi/10.1161/ST…
21/🧵
1- nejm.org/doi/full/10.10…
2- @rishikumarmd Post on LVADs rk.md/2015/what-left…
3- ahajournals.org/doi/10.1161/ST…
21/🧵
@EmoryCCC @sigman_md @EmoryCritAPP @EmoryNeuroCrit @criticalbeansmd @caseyalbin @drdangayach @Aartisarwal @NaomiNiznick @EmmGeezee @JimmySuhMD @MedTweetorials @emcrit @Gradydoctor @laxswamy @InternAtWork @CardioNerds @Capt_Ammonia @AubreyantMD @emory_heart
22/22
22/22
@DrManiCTSurgery @MaanJokhadar @JackieKraft4 @feras_akbik @clhallmd @neuro_intensive @CajalButterfly
• • •
Missing some Tweet in this thread? You can try to
force a refresh








