Which statement is correct with regards to the use of diuretics in #HeartFailure with congestion?
Short #Tweetorial on how to use diuretics in heart failure (1/9).
#Cardiotwitter #Cardiology #FOAMed #Cardiorenal #MedEd #MedTwitter #Nephrology #ADVOR #HeartFailure2022 #HFA_ESC
Short #Tweetorial on how to use diuretics in heart failure (1/9).
#Cardiotwitter #Cardiology #FOAMed #Cardiorenal #MedEd #MedTwitter #Nephrology #ADVOR #HeartFailure2022 #HFA_ESC
Door to ‘diuretic’ time: earlier administration of loop diuretics is associated with improved outcomes independent of HF severity (2/9).
jacc.org/doi/abs/10.101…
jacc.org/doi/abs/10.101…

The first dose of the loop diuretic should be 40 mg furosemide (=1 mg bumetanide) in diuretic naïve and twice the home dose in patients on loop diuretic (3/9). 

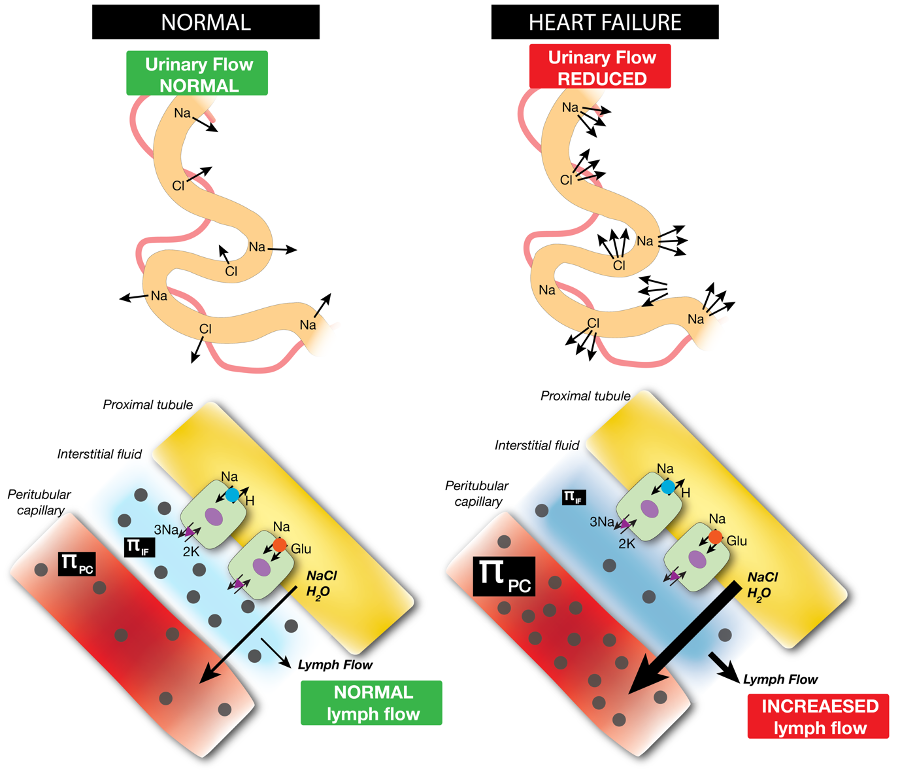
Diuretics work for 6-8 hours so evaluate the effect within hours after administration. The next dose should be individualized according to the natriuretic and/or diuretic response which should be Na > 50-70 meq/l and/or volume > 100-150 ml/hour (4/9). 

In case of ‘good diuretic – natriuretic’ response: continue similar dose every 12 hours until decongested. In case of ‘suboptimal diuretic – natriuretic’ response: double the dose immediately and evaluate again. Maximum dose furosemide is 200 mg IV bolus, three times daily (5/9). 

After 24 hours: When urinary output is > 3-4 l/ 24 hours, continue current dose regimen. When < 3-4 l/24 hours, diuretic escalation is warranted (6/9). 

Look out for the worldwide #ENACTHF study, led by @JeroenDauw
and PUSH-AHF, led by @jozinetm who are testing this algorithm (8/9).
onlinelibrary.wiley.com/doi/10.1002/eh…
onlinelibrary.wiley.com/doi/10.1002/ej…
@CpaolaParedes
@drdianebarker
@GonBarge
@rdelaespriella
@ChristophSinni1
@MartaCoboMarcos
and PUSH-AHF, led by @jozinetm who are testing this algorithm (8/9).
onlinelibrary.wiley.com/doi/10.1002/eh…
onlinelibrary.wiley.com/doi/10.1002/ej…
@CpaolaParedes
@drdianebarker
@GonBarge
@rdelaespriella
@ChristophSinni1
@MartaCoboMarcos

Please have a look at this very practical HFA position statement on diuretic treatment of HF with congestion (9/9).
onlinelibrary.wiley.com/doi/full/10.10…
@WilsonTangMD @FH_Verbrugge @petra_nijst @PieterMartensMD @kevin_damman @AlexMebazaa @berzin78 @MarcoMetra @Filippatos @robmentz
onlinelibrary.wiley.com/doi/full/10.10…
@WilsonTangMD @FH_Verbrugge @petra_nijst @PieterMartensMD @kevin_damman @AlexMebazaa @berzin78 @MarcoMetra @Filippatos @robmentz

• • •
Missing some Tweet in this thread? You can try to
force a refresh