1/ Welcome back to another edition of #TweetorialTuesday from the @MedEdTwagTeam. Special S/O to our #MedEd & #MedTwitter friends!
Over the last two weeks we have laid out the WHY and the WHAT of teaching communication. Today is the HOW. Let’s go!
Over the last two weeks we have laid out the WHY and the WHAT of teaching communication. Today is the HOW. Let’s go!

2/ For refreshers on the WHY and WHAT, check out these previous threads from:
@JenniferSpicer4 (WHY) –
@GStetsonMD (WHAT) –
@JenniferSpicer4 (WHY) –
https://twitter.com/JenniferSpicer4/status/1506358660766867460
@GStetsonMD (WHAT) –
https://twitter.com/GStetsonMD/status/1508815468798398478
3/ And like the previous threads, much of this content comes from this book (Chapter 16 for this thread) by @DrCalvinChou & @LauraCooleyPhD of @ACHonline. It is a foundational book that is extremely readable and applicable. Well worth your time: CommunicationRx.org 
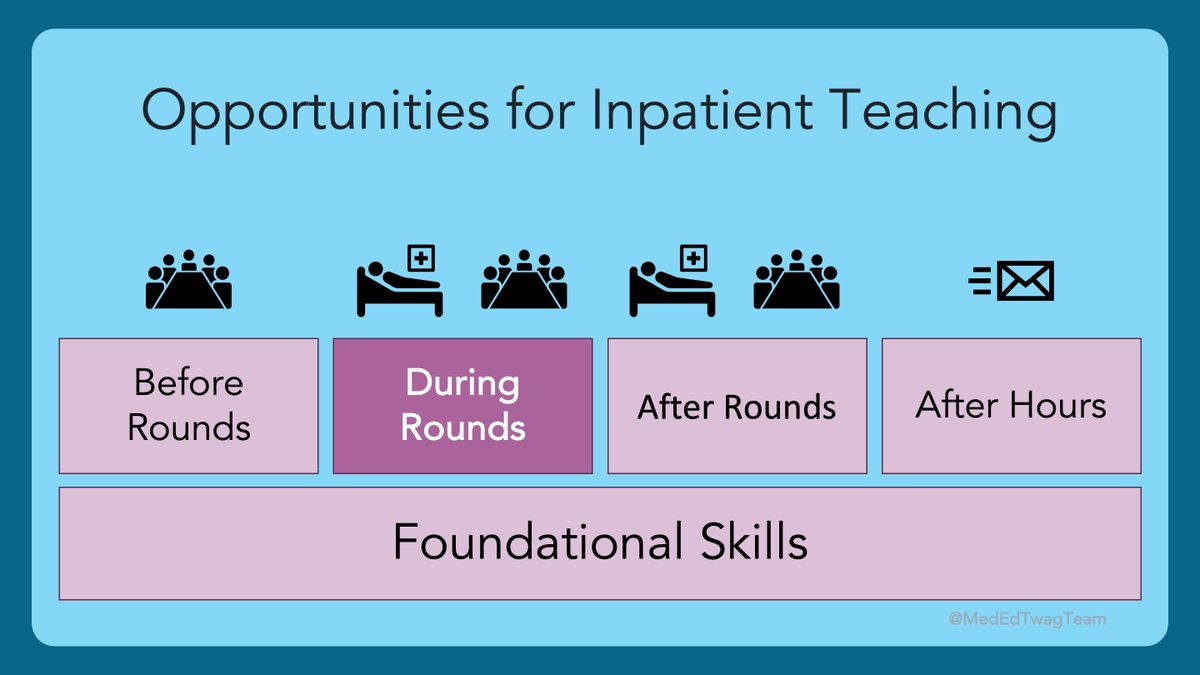
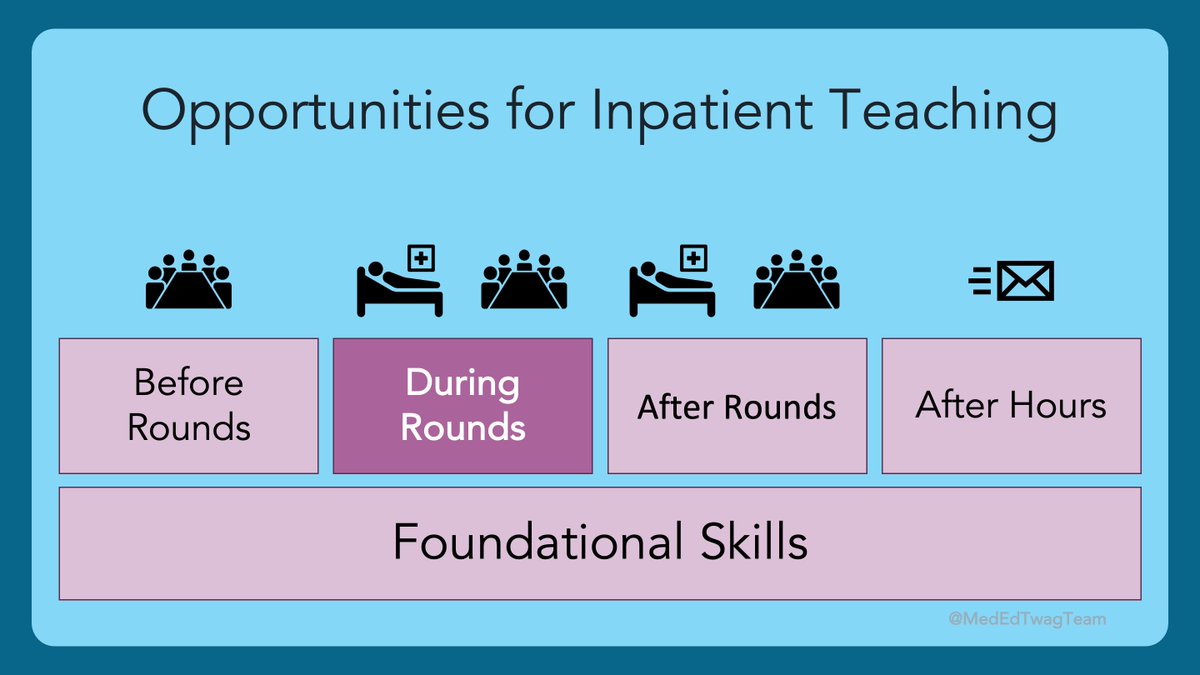
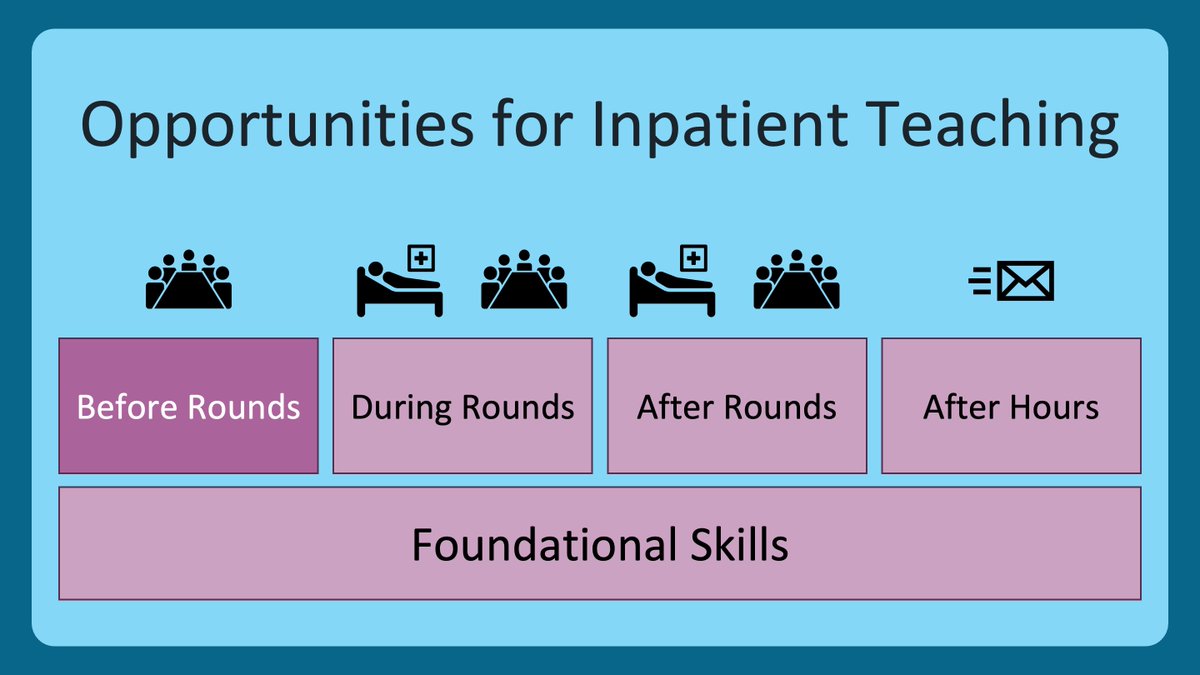
4/ We are still in this “during rounds” section of our inpatient teaching block. When teaching and learning communication skills, rounds is the perfect time to put in some meaningful practice. 

5/ Why is rounds perfect?
This review article identified role play, feedback, and small group discussion as the most effective ways to teach communication skills. Swap real patients for role plays, and does that sound like rounds to anyone else?
pubmed.ncbi.nlm.nih.gov/20673620/
This review article identified role play, feedback, and small group discussion as the most effective ways to teach communication skills. Swap real patients for role plays, and does that sound like rounds to anyone else?
pubmed.ncbi.nlm.nih.gov/20673620/

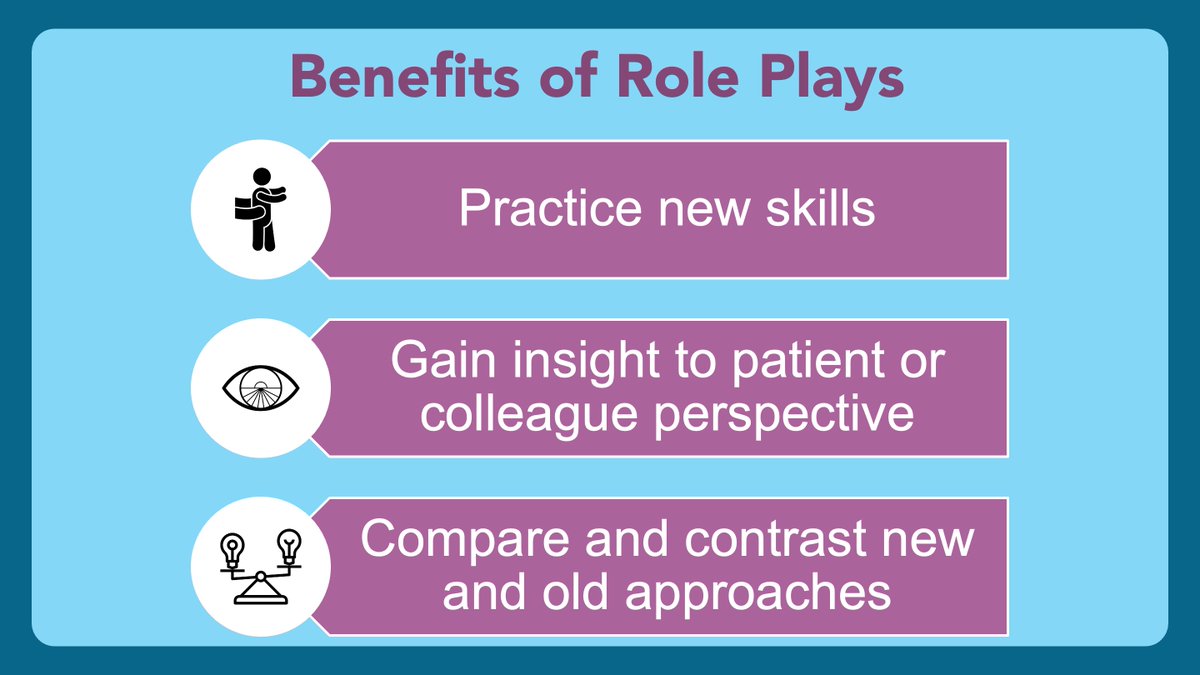
6/ However, actual role play can also be used to practice a skill before heading into a patient encounter, or after an encounter where there were missed opportunities to provide empathy, for example. 
7/ So, whether it is with a real patient, or just within the team in a role play, it is important that your learners feel safe and supported. Here are ways to facilitate this:
1⃣Let them know they have a coach in their corner
2⃣Review the skills that they will practice
1⃣Let them know they have a coach in their corner
2⃣Review the skills that they will practice

8/ More guiding principles:
3⃣Agree on a sign that the learner can use to call you in to take over the conversation
4⃣Check in with the participant so they can reflect on their own experience
3⃣Agree on a sign that the learner can use to call you in to take over the conversation
4⃣Check in with the participant so they can reflect on their own experience

9/ Last set of principles here:
5⃣Providing meaningful feedback is key to a useful activity
6⃣Make sure your learner gets another chance to use the skill with you observing
For more on effective feedback, see these threads: twitter.com/i/events/13632…
5⃣Providing meaningful feedback is key to a useful activity
6⃣Make sure your learner gets another chance to use the skill with you observing
For more on effective feedback, see these threads: twitter.com/i/events/13632…

10/ I also want to put in a plug for role MODELing instead of role PLAY. I am big into letting the learners run the show, but if there is a particularly difficult conversation, or maybe a super routine one, it can be really powerful to ask the team to be observers. 

11/ So, the key to effective teaching of communication skills is creating safe opportunities to practice. Didactic activities are good for transmitting information but have little effect on attitudes and behaviors. Learners need direct observation and feedback. 

12/ Thanks for joining us for this 3-week foray into communication. Next week, @JenniferSpicer4 will help us make sure every learner stays engaged on rounds.
Follow her, myself, and the other @MedEdTwagTeam members (@ChrisDJacksonMD & @YihanYangMD) so you don’t miss a thing!
Follow her, myself, and the other @MedEdTwagTeam members (@ChrisDJacksonMD & @YihanYangMD) so you don’t miss a thing!
• • •
Missing some Tweet in this thread? You can try to
force a refresh