What to do if the eGFR drops from 50 to 42 ml/min/m2 during decongestive therapy in acute #HeartFailure ?
Short #Tweetorial on worsening renal function (WRF) (1/9).
#Cardiotwitter #Cardiology #FOAMed #Cardiorenal #MedEd #MedTwitter #Nephrology #ADVOR #HeartFailure2022 #HFA_ESC
Short #Tweetorial on worsening renal function (WRF) (1/9).
#Cardiotwitter #Cardiology #FOAMed #Cardiorenal #MedEd #MedTwitter #Nephrology #ADVOR #HeartFailure2022 #HFA_ESC
There is an underappreciated risk of poor outcome in heart failure patients discharged with ongoing congestion and WRF (2/9).
Pivotal paper of @MarcoMetra ahajournals.org/doi/10.1161/ci…
Pivotal paper of @MarcoMetra ahajournals.org/doi/10.1161/ci…

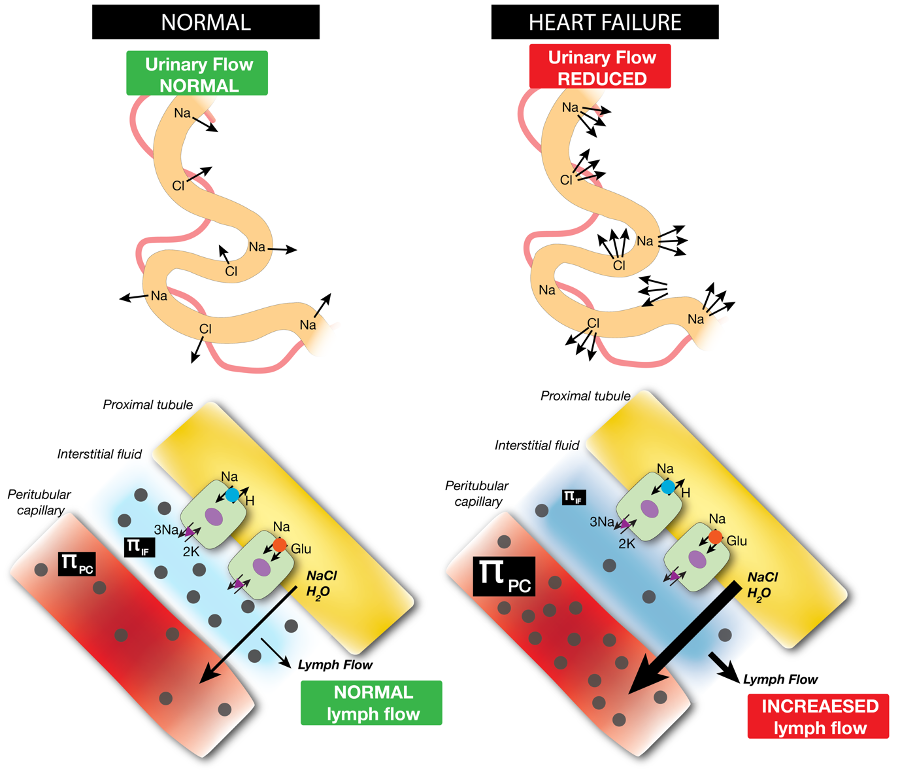
Appropriate and thorough decongestion is class I recommendation in HFA-ESC guidelines so DON'T stop decongestive efforts during WRF (3/9).
academic.oup.com/eurheartj/arti…
academic.oup.com/eurheartj/arti…

Clinical scenario 1 = assess diuretic response -> if OK: continue similar decongestive efforts (=pseudo-WRF) (4/9). 

Clinical scenario 2 = assess diuretic response -> if poor -> assess CVP + TTE + measure intra-abdominal pressure (IAP) -> consider paracentesis if IAP ↑ secondary to ascites (5/9) 
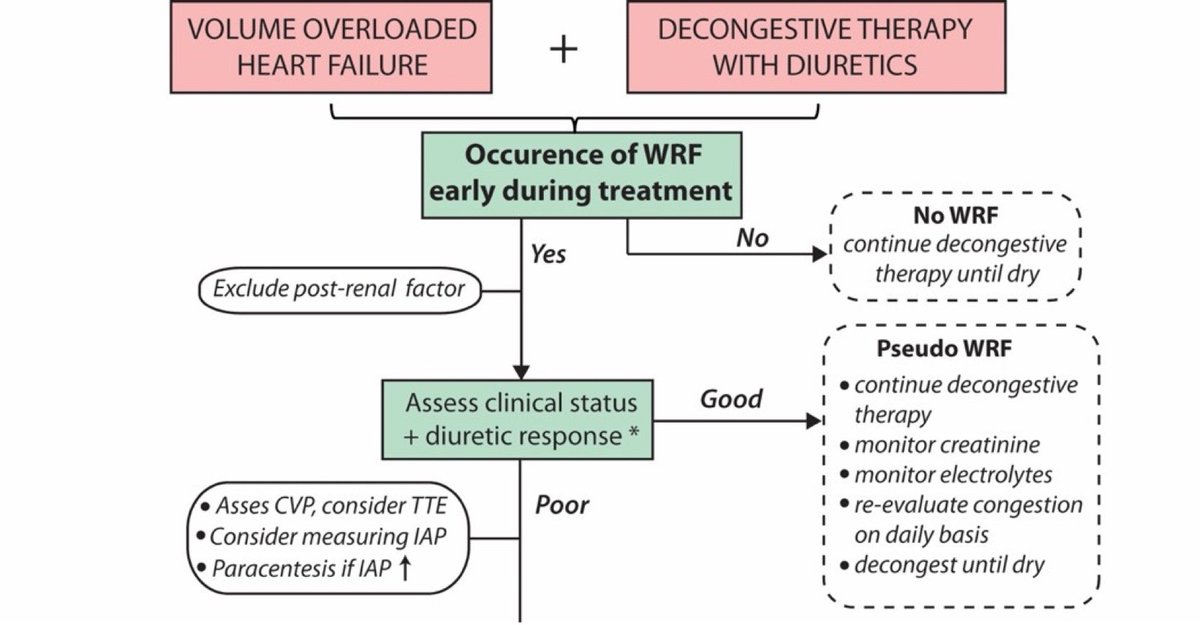
Clinical scenario 3: check for hypoperfusion (which is extremely rare) -> if hypoperfusion: consider mechanical circulatory support or inotropic agents to optimize hemodynamic status (6/9). 

Clinical scenario 4: check for hypoperfusion -> if no hypoperfusion: increase diuretic intensity and consider IV vasodilators (7/9). 

In parallel: continue and even upitrate neurohumoral blockers as diuretic efficacy is increased despite lower blood pressure and WRF, however caution if serum creatinine increase is too high (8/9)
ahajournals.org/doi/10.1161/CI…

ahajournals.org/doi/10.1161/CI…


Have a look at HFA position statement on WRF during diuretic treatment in HF (9/9).
onlinelibrary.wiley.com/doi/full/10.10…
@WilsonTangMD @FH_Verbrugge @petra_nijst @PieterMartensMD @JeroenDauw @kevin_damman @jozinetm @AlexMebazaa @berzin78 @robmentz @ISNkidneycare @HillLoreena @MarcoMetra
onlinelibrary.wiley.com/doi/full/10.10…
@WilsonTangMD @FH_Verbrugge @petra_nijst @PieterMartensMD @JeroenDauw @kevin_damman @jozinetm @AlexMebazaa @berzin78 @robmentz @ISNkidneycare @HillLoreena @MarcoMetra

• • •
Missing some Tweet in this thread? You can try to
force a refresh