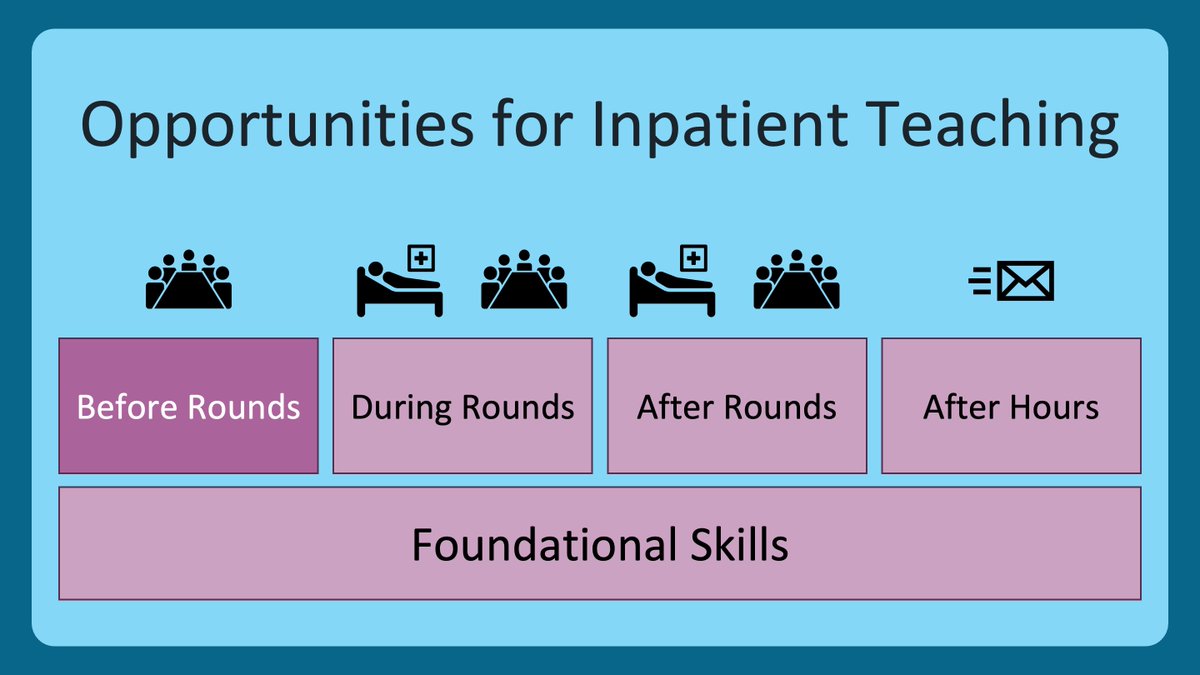
1/ You just admitted a patient with some really interesting pathology. You want to teach about it tomorrow on rounds. You know it is gonna be a busy day. What’s the plan?
Welcome back to #TweetorialTuesday from the @MedEdTwagTeam. Special S/O to our #MedEd & #MedTwitter friends!
Welcome back to #TweetorialTuesday from the @MedEdTwagTeam. Special S/O to our #MedEd & #MedTwitter friends!

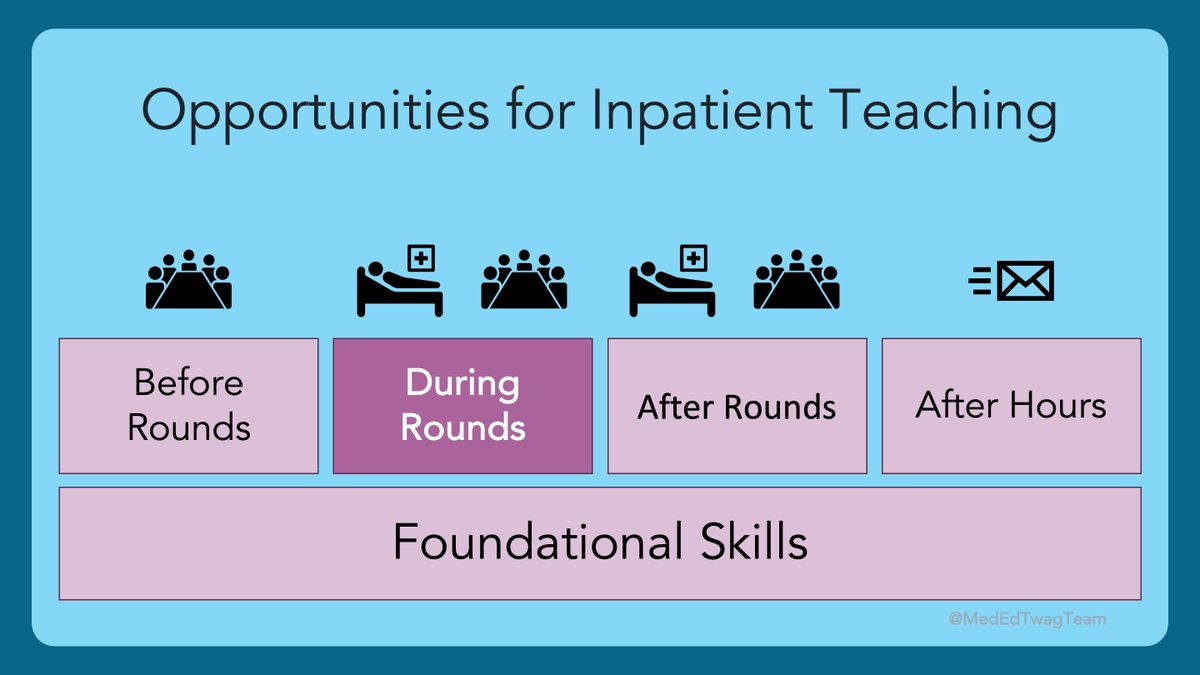
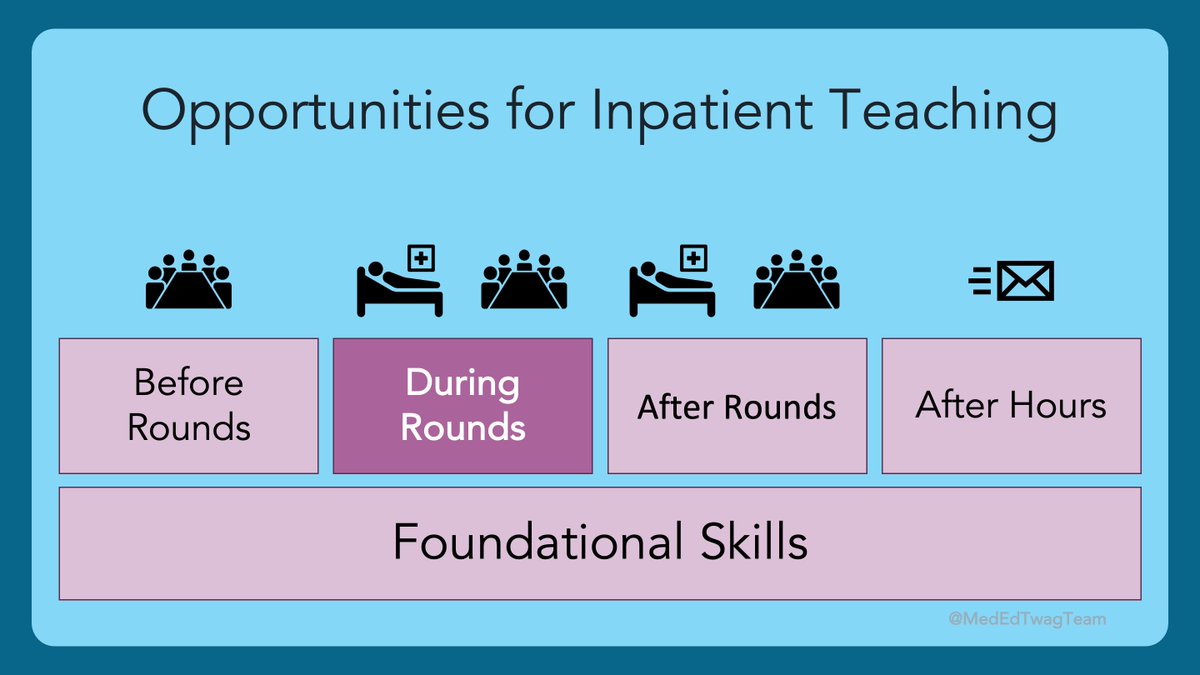
2/ We are still in this “during rounds” section of our inpatient teaching block. Rounds are the CLASSIC time to drop pearls. But, doing it well takes thought and preparation. 

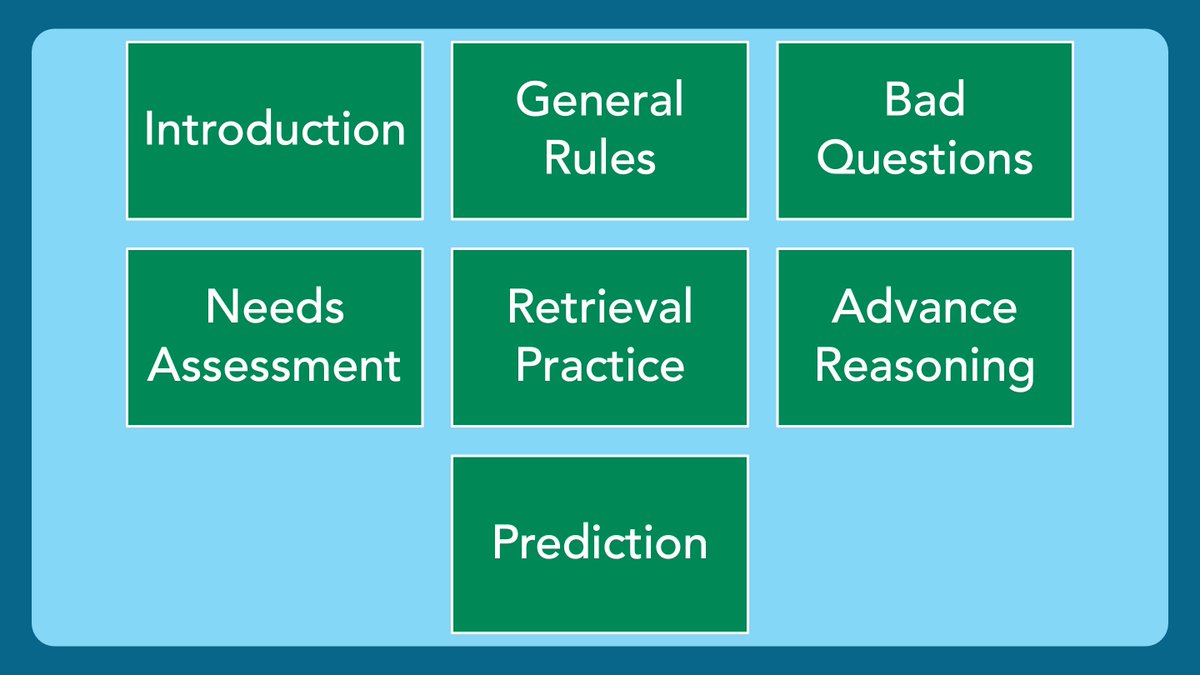
3/ What does it mean to “drop pearls”? It refers to pearls of wisdom, and many of us think of some stately professor emeritus waxing poetic in a case conference.
But check out this definition here:
But check out this definition here:

4/ What I like about the previous definition is “a wise word or statement.” This suggests that the ideal approach to dropping pearls is short, pithy, and to the point. That is not always how “dropping pearls” goes in my experience. 

5/ What I often see when a student, intern, resident, or junior faculty gets excited about a topic is they start teaching without a clear plan of what salient points they want learners to take away. It’s good information. it just isn’t organized, grounded, primed or timed well. 

6/ Being able to create learning objectives is key to taking excitement about a topic and organizing it into effective and meaningful teaching. We have talked about learning objectives before. Check out the previous thread here:
https://twitter.com/GStetsonMD/status/1442894291840299016
7/ Next, you need to grab the audience’s attention. Tell them the learning objective you plan to meet and why that is relevant to the patient you are seeing on rounds. This grounds the content and primes the learners’ brains for incorporating the new information.
8/ Lastly, we are on rounds. Time is incredibly valuable. Being succinct & clear in what you are teaching is key to respecting everyone’s time, which allows them to focus on you. Decide how long it will take to teach your pearl (shorter is better) & announce it before you start!
9/ When learners don’t know how long learning is going to take, they zone out FAST! If you tell them, “I’ve got 2 minutes of teaching on MRSA bacteremia,” they’re probably thinking, “2 minutes?!? I can spare 2 minutes,” and you get undivided attention. But, you must stick to it!
10/ It will surprise no one on #MedEd Twitter that @LekshmiMD modeled this perfectly. Picture baby intern Geoff on Dr. Santhosh’s team when she was a junior resident. She did something she called Two-Minute Teaching at the Top (or TTT). Here is what she did and why it worked: 

11/ Thanks for joining us to pick up some pearls about dropping them. Next week, @ChrisDJacksonMD is gonna keep this pearl train going but with an Evidence-Based Medicine (EBM) twist.
And make sure you are following the rest of the @MedEdTwagTeam @JenniferSpicer4 @YihanYangMD!
And make sure you are following the rest of the @MedEdTwagTeam @JenniferSpicer4 @YihanYangMD!
• • •
Missing some Tweet in this thread? You can try to
force a refresh