#Medtwitter, last week I posted about a talk I gave on teaching #clinicalreasoning
As promised, the accompanying #tweetorial
Come explore with me!
1/10

As promised, the accompanying #tweetorial
Come explore with me!
1/10
https://twitter.com/AnandJag1/status/1519499322236178433?s=20&t=XFdniGzBgA8tQ3tB4LcW6g

I described a gap between DOING and TEACHING reasoning
All of us DO reasoning every day
TEACHING what we DO is hard unless we
✔️have vocabulary to describe it
✔️know how to describe a process
✔️are ok being vulnerable in front of others
2/10
All of us DO reasoning every day
TEACHING what we DO is hard unless we
✔️have vocabulary to describe it
✔️know how to describe a process
✔️are ok being vulnerable in front of others
2/10

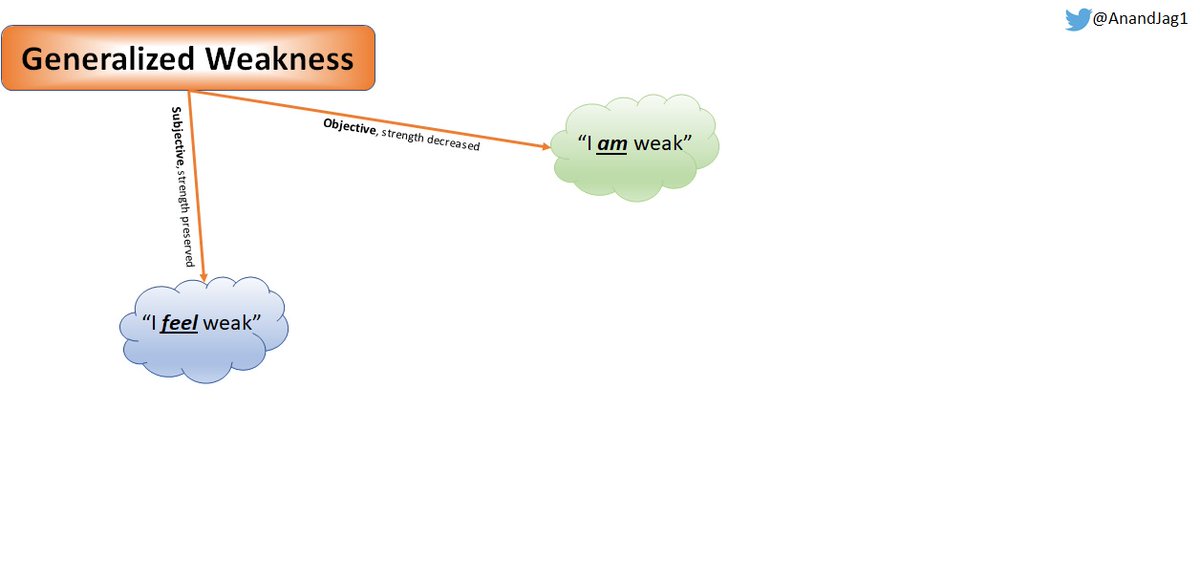
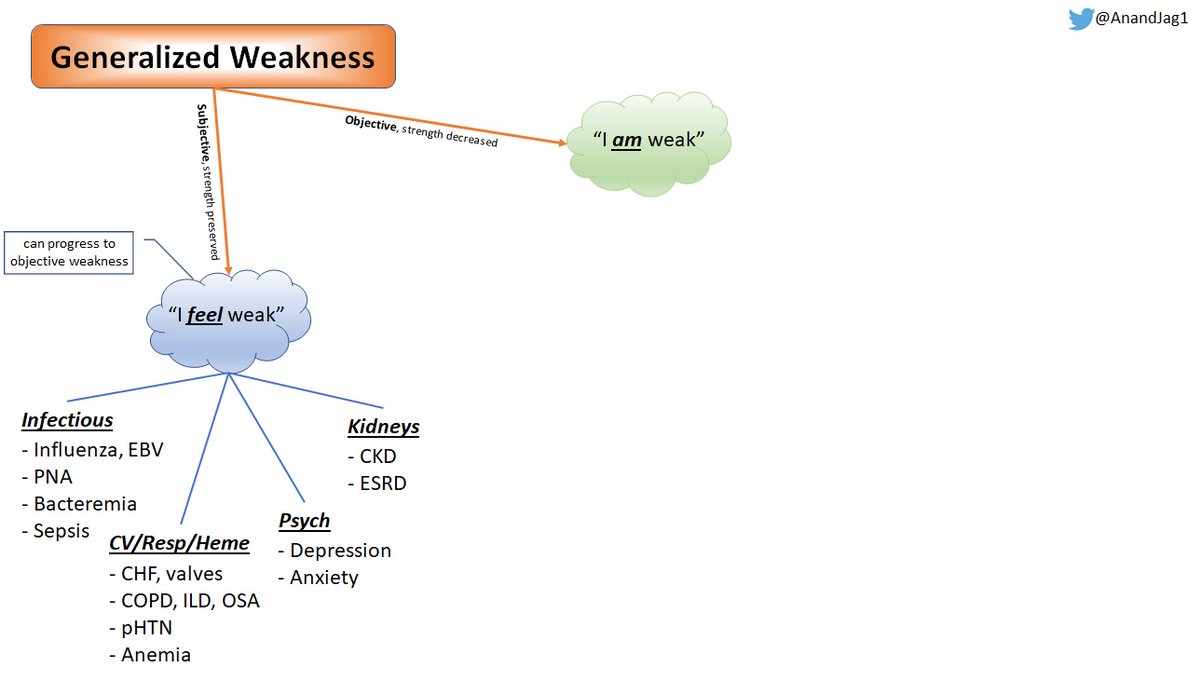
How do we make an invisible process (reasoning), visible?
Step 1: use specific words to describe steps to the cognitive process:
Problem representation
Schema
Illness scripts
Speaking these words signals their importance to your learners - use them!
3/10
Step 1: use specific words to describe steps to the cognitive process:
Problem representation
Schema
Illness scripts
Speaking these words signals their importance to your learners - use them!
3/10

Step 2: engage in a Cognitive Apprenticeship
An evolution of the traditional apprenticeship, CA emphasizes narrated thinking in many forms to develop reasoning skills
Not unique to medicine, but applicable
Many techniques within CA - these 3 are money
4/10
An evolution of the traditional apprenticeship, CA emphasizes narrated thinking in many forms to develop reasoning skills
Not unique to medicine, but applicable
Many techniques within CA - these 3 are money
4/10

Applied to teaching reasoning:
💥Thinking aloud shows how reasoning happens
💥Coaching lets you observe and give real-time feedback
💥Reflection helps build plans for improvement
🎩@jackpenner for teaching me🙏🌹
💡more on CA: pubmed.ncbi.nlm.nih.gov/25800294/
5/10
💥Thinking aloud shows how reasoning happens
💥Coaching lets you observe and give real-time feedback
💥Reflection helps build plans for improvement
🎩@jackpenner for teaching me🙏🌹
💡more on CA: pubmed.ncbi.nlm.nih.gov/25800294/
5/10
Step 3: Intellectual Streaking!!
Drs. Bearman and Molloy teach that I.S. is the way we expose uncertainty to our learners to model growth
@LiangRhea made me aware of this term 🙏🌹
@CPSolvers builds their culture around it ("I don't know!")❤️
6/10
Drs. Bearman and Molloy teach that I.S. is the way we expose uncertainty to our learners to model growth
@LiangRhea made me aware of this term 🙏🌹
@CPSolvers builds their culture around it ("I don't know!")❤️
6/10

Becoming comfortable with being UNcomfortable is how we go from projecting our uncertainty on our learners to showing learners how WE find and fill our gaps in knowledge and reasoning
7/10
7/10

The gap between DOING and TEACHING reasoning is understandably large, but by remembering that reasoning is a process, we can take steps to define, shrink, and even bridge that gap
8/10
8/10

Taking a page from @gradydoctor's book, so much gratitude for these humans for giving me opportunity and trust, role-modeling excellence, and teaching me new things. You are all gems 🙏🌹❤️
9/10
9/10

For more, including inspiration behind the title and some worked examples, I'm happy to give the full version of this talk in-person or remotely!
Thank you, #Medtwitter!
10/10
Thank you, #Medtwitter!
10/10

• • •
Missing some Tweet in this thread? You can try to
force a refresh