A traumatic but necessary read 👇
Thanks to @TheBMA, @CNagpaul @ProfEmer @martinmckee et al
But given what's happened today with the email from @SMHopkins & @Thomas_Waite, I need to share a FOI response that seems now to have found a suitable home
/🧵
bma.org.uk/media/5644/bma…
Thanks to @TheBMA, @CNagpaul @ProfEmer @martinmckee et al
But given what's happened today with the email from @SMHopkins & @Thomas_Waite, I need to share a FOI response that seems now to have found a suitable home
/🧵
bma.org.uk/media/5644/bma…
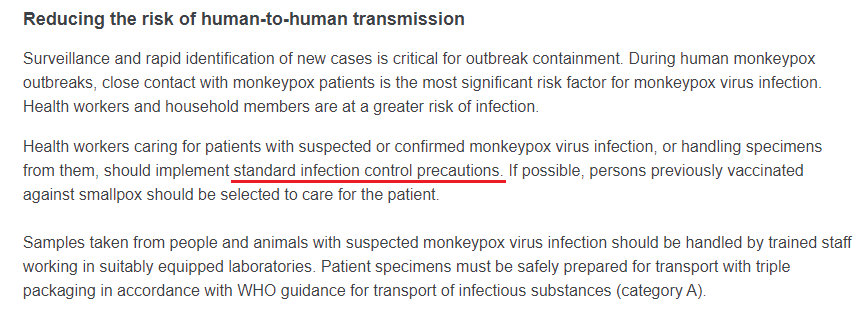
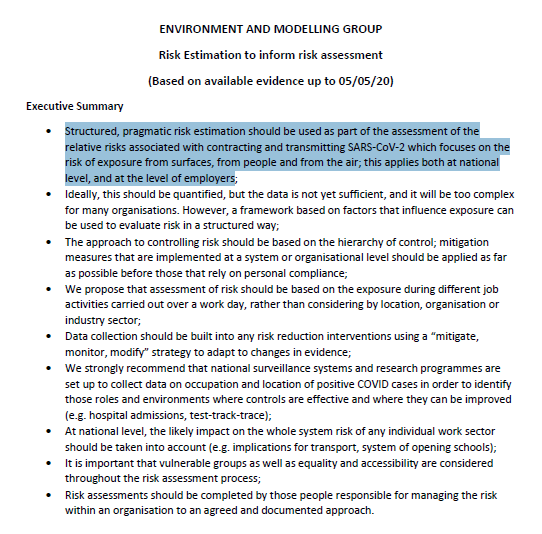
I need to speak into the IPC guidance narrative presented:
'throughout February & early March 2020 IPC guidance was piecemeal and of little practical value'
'Mid-March 2020 saw the release of the first iteration of more comprehensive IPC guidance for healthcare workers'
/2
'throughout February & early March 2020 IPC guidance was piecemeal and of little practical value'
'Mid-March 2020 saw the release of the first iteration of more comprehensive IPC guidance for healthcare workers'
/2

Respectfully, this may create the impression that IPC guidance IMPROVED comparing Feb/early Mar & mid-March
But the evidence below proves that only this early IPC guidance (here, reflecting UK policy via the Health Protection Scotland archive, HPS) was truly life-saving
/3
But the evidence below proves that only this early IPC guidance (here, reflecting UK policy via the Health Protection Scotland archive, HPS) was truly life-saving
/3
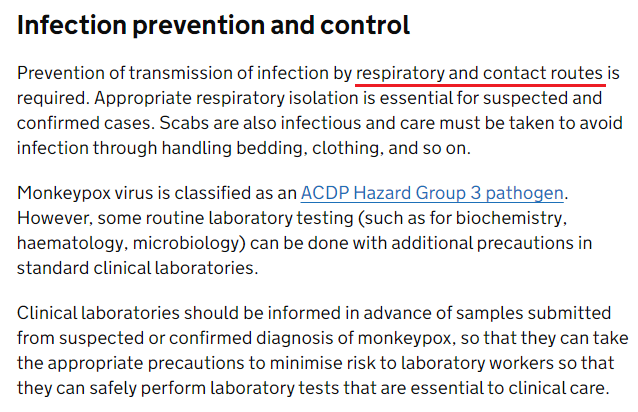
From the HPS archive, 5th Mar 2020
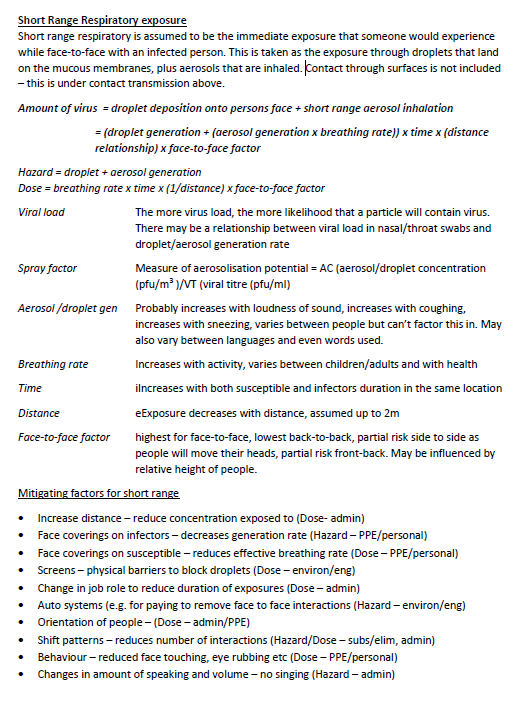
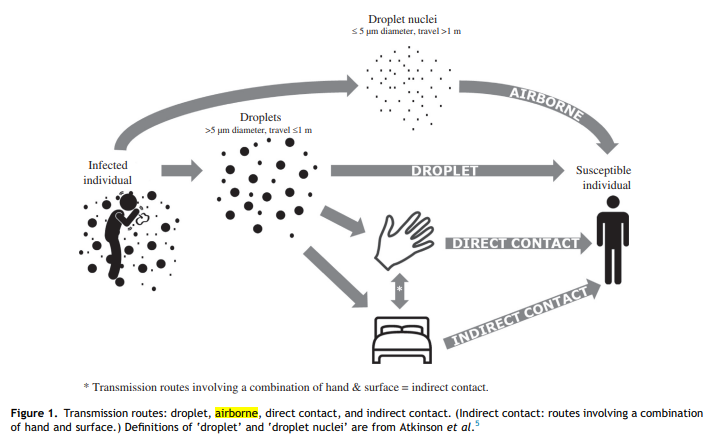
'COVID-19 is currently classified as a High Consequence Infectious Diseases (HCID) spread by respiratory droplets in addition to contact routes & REQUIRE AIRBORNE PRECAUTIONS.'
[CAPS for emphasis]
Plus...
/4

'COVID-19 is currently classified as a High Consequence Infectious Diseases (HCID) spread by respiratory droplets in addition to contact routes & REQUIRE AIRBORNE PRECAUTIONS.'
[CAPS for emphasis]
Plus...
/4


5th Mar 2020
'This document outlines the infection prevention & control advice for healthcare workers who may be involved in receiving, assessing & caring for patients, within acute healthcare settings, who are a POSSIBLE OR CONFIRMED case.'
/5
'This document outlines the infection prevention & control advice for healthcare workers who may be involved in receiving, assessing & caring for patients, within acute healthcare settings, who are a POSSIBLE OR CONFIRMED case.'
/5

'If a contact of a confirmed case develops a respiratory illness & is hospitalised, then this guidance should be followed until results of testing are available.
The precautionary principle should be applied for all novel or emerging respiratory pathogens of high consequence
/6
The precautionary principle should be applied for all novel or emerging respiratory pathogens of high consequence
/6

...when the mode of transmission is incompletely determined. AIRBORNE PRECAUTIONS (including the use of correctly fitted FFP3 respirators) should be applied for ALL patients admitted with SUSPECTED OR CONFIRMED COVID-19.’
Piecemeal? Of little practical value?
/7
Piecemeal? Of little practical value?
/7

OK, so that was 5th Mar
hps.scot.nhs.uk/media/1950/inf…
Next HPS version archived: 10th Mar
hps.scot.nhs.uk/media/1951/inf…
Any guesses as to what new data helped inform IPC guidance changes in the 2 full working days between these dates?
I'm getting ahead of myself; guidance changes first
/8
hps.scot.nhs.uk/media/1950/inf…
Next HPS version archived: 10th Mar
hps.scot.nhs.uk/media/1951/inf…
Any guesses as to what new data helped inform IPC guidance changes in the 2 full working days between these dates?
I'm getting ahead of myself; guidance changes first
/8
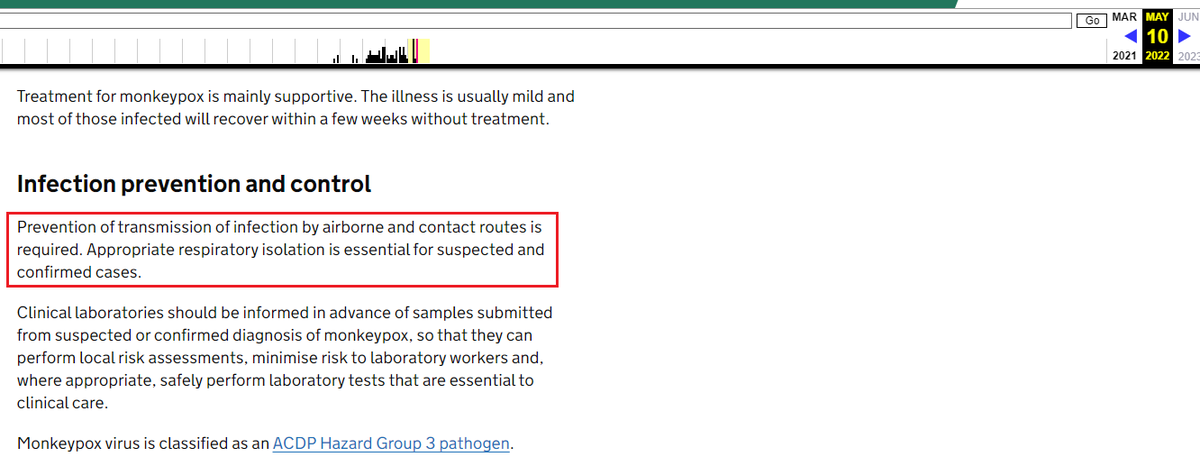
10th Mar 2020, opening section:
'COVID-19 is currently classified as a High Consequence Infectious Diseases (HCID) spread by respiratory droplets in addition to contact routes & require airborne precautions when in a High Risk AGP hot spot[1] or when undertaking AGPs'
😲
/9

'COVID-19 is currently classified as a High Consequence Infectious Diseases (HCID) spread by respiratory droplets in addition to contact routes & require airborne precautions when in a High Risk AGP hot spot[1] or when undertaking AGPs'
😲
/9


10th Mar 2020, next section:
The entire paragraph regarding the precautionary principle is AWOL
Pic 1: 5th Mar
Pic 2: 10th Mar
@DavidShukman @trishgreenhalgh @ProfEmer @CNagpaul @SMHopkins @Thomas_Waite @Lisaritchie111 @PeterHorby
/10

The entire paragraph regarding the precautionary principle is AWOL
Pic 1: 5th Mar
Pic 2: 10th Mar
@DavidShukman @trishgreenhalgh @ProfEmer @CNagpaul @SMHopkins @Thomas_Waite @Lisaritchie111 @PeterHorby
/10


Would you like to know what new data was so compellingly AGAINST airborne transmission of SARS2 that the previously mandated FFP3 for suspected/confirmed cases & the precautionary principle could be completely dismissed?
I asked, & got a FOI response
/11
I asked, & got a FOI response
/11
FOI response
I received two clips from PDFs in draft mode - names of those responsible for the edits redacted
Edits in next tweet...
/13
I received two clips from PDFs in draft mode - names of those responsible for the edits redacted
Edits in next tweet...
/13

No new manuscripts, no mechanistic proof of pure splash droplet & contact transmission, no modelling data...nothing to support these incremental changes AWAY from universal FFP3 - per SARS2 - AWAY from the precautionary principle, & TOWARDS certain exposure for non-ICU staff
/14

/14


My separate FOI requesting confirmation of who had governance oversight for sign-off for these documents was rejected
I was told 'Public Health Consultants' were responsible
But will you allow me to speculate, just a bit?
I promise I won't be defamatory
/15
I was told 'Public Health Consultants' were responsible
But will you allow me to speculate, just a bit?
I promise I won't be defamatory
/15
For this you need the NERVTAG minutes:
9th April 2020, meeting 13
NERVTAG chair described responsibilities: '...watching brief on new evidence & updating the committee at the meetings.
IPC measures - LR'
Lisa Ritchie, Head of IPC at NHSE/I
/16
app.box.com/s/3lkcbxepqixk…
9th April 2020, meeting 13
NERVTAG chair described responsibilities: '...watching brief on new evidence & updating the committee at the meetings.
IPC measures - LR'
Lisa Ritchie, Head of IPC at NHSE/I
/16
app.box.com/s/3lkcbxepqixk…
At meeting 13, Lisa Ritchie was described as an 'Invited expert'
But at NERVTAG meetings 3-9, 28th Jan - 13th Mar 2020, Lisa Ritchie's affiliation every single time is given as 'HPS'
/17
But at NERVTAG meetings 3-9, 28th Jan - 13th Mar 2020, Lisa Ritchie's affiliation every single time is given as 'HPS'
/17

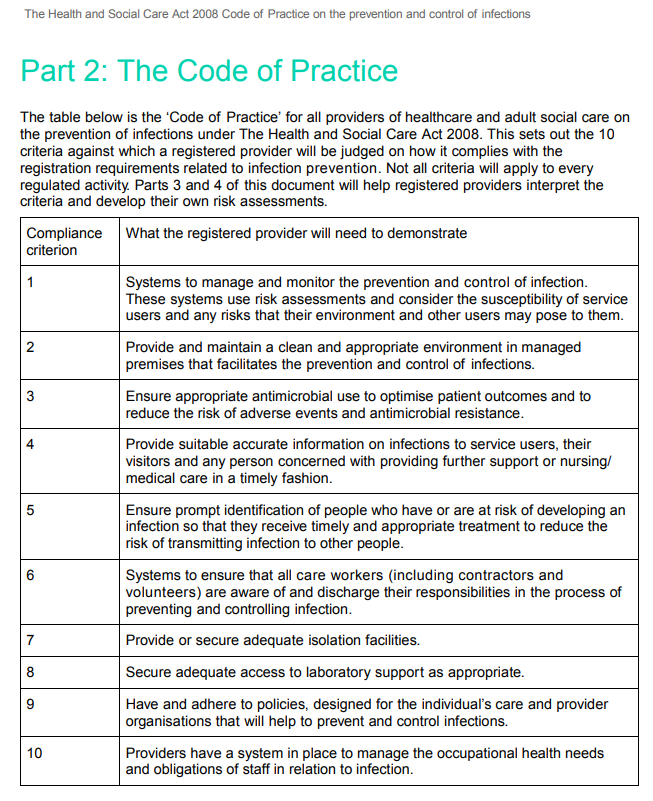
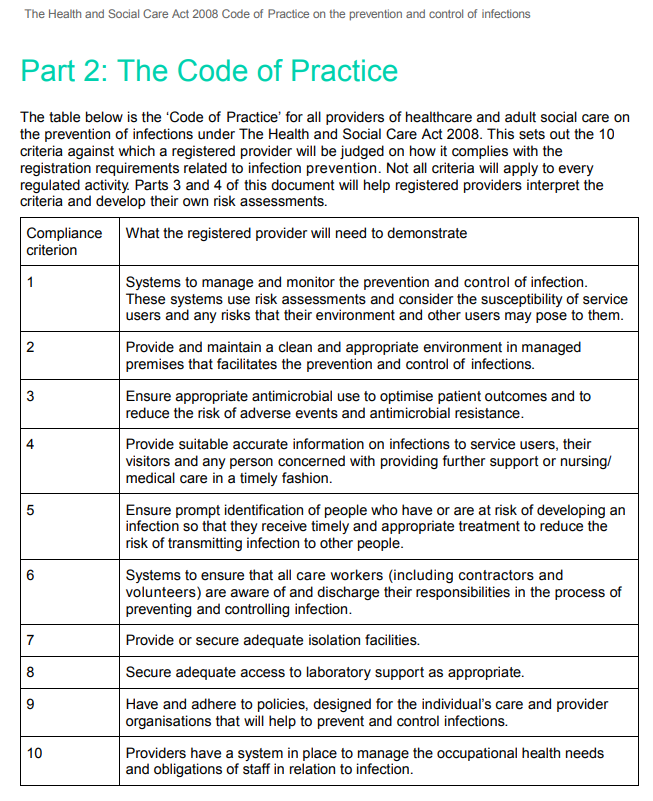
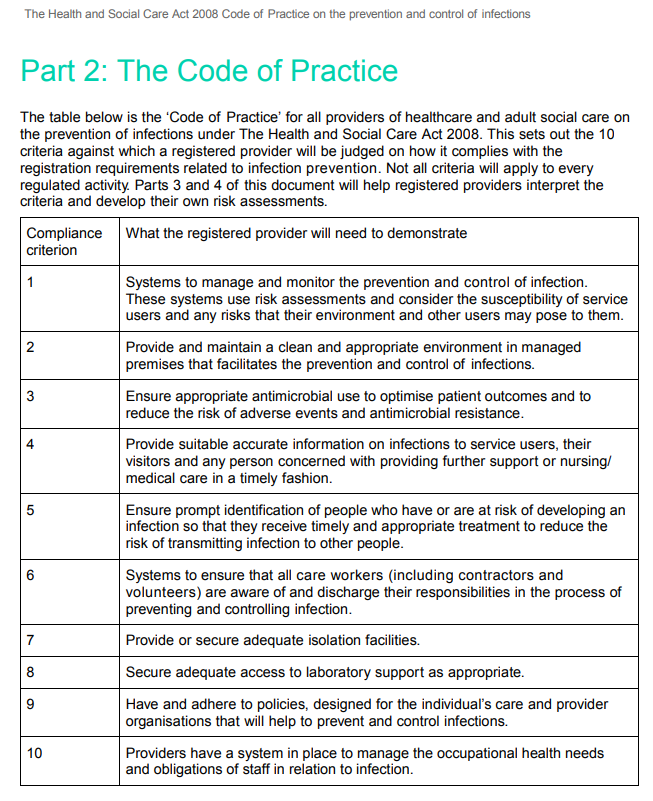
Even a casual reader of these early March 2020 minutes will realise that there was a catastrophic shortfall in RPE
Evidence?
6th Mar: '2.1 PHE were asked to update the secondary care guidance in light of the CMO stern earlier in the week'
Suspected cases now given FRSM
/18
Evidence?
6th Mar: '2.1 PHE were asked to update the secondary care guidance in light of the CMO stern earlier in the week'
Suspected cases now given FRSM
/18
'2.4 WSL was forwarded some emails from PHE on this topic that suggested the main thrust for this change was around FFP3 stock where a lot of the stock is being used up for fit-testing & there are concerns that there may not be enough FFP3 stock for use later on...'
/19
/19

& @DavidShukman uncovered the truth of airborne HCID declassification, 13th Mar 2020; equally non-evidence based & borne of necessity to provide a 'scientific veneer' to downgraded PPE guidance for non-ICU HCWs
You were right to worry @doctor_oxford
bbc.co.uk/news/health-55…
You were right to worry @doctor_oxford
bbc.co.uk/news/health-55…
But HPS staff - including Lisa Ritchie - didn't make these IPC guidance changes in isolation
They received the affirmation of NERVTAG
Chaired by @PeterHorby
& in the 'more comprehensive IPC guidance' from mid-Mar, NERVTAG even threw their weight behind the PPE downgrade
/21
They received the affirmation of NERVTAG
Chaired by @PeterHorby
& in the 'more comprehensive IPC guidance' from mid-Mar, NERVTAG even threw their weight behind the PPE downgrade
/21

'The predominant modes of transmission are assumed to be droplet & contact'
FALSE ASSUMPTION, contradicted by JVT & Lisa Ritchie's own 2013 publication on RPE
Dear journalists, please check my working, if you think this is newsworthy? 💙
And...
/22

FALSE ASSUMPTION, contradicted by JVT & Lisa Ritchie's own 2013 publication on RPE
Dear journalists, please check my working, if you think this is newsworthy? 💙
And...
/22


'In light of the above, the Department of Health and Social Care’s New & Emerging Respiratory Virus Threat Assessment Group (NERVTAG) have recommended that airborne precautions should be implemented at all times in clinical areas considered AGP ‘hot spots’...
/23

/23


'In other areas a fluid-resistant (Type IIR) surgical mask (FRSM) is recommended; all general ward staff, community, ambulance & social care staff should wear an FRSM for close patient contact (within 1 metre), unless performing an AGP...'
Thanks for caring, NERVTAG
/24

Thanks for caring, NERVTAG
/24


So why did the UK have such a catastrophic shortfall in RPE that ALL non-ICU healthcare workers were effectively thrown under a bus?
Why the planning shortfall?
Well, at least in part, we have NERVTAG to thank for this too
/25
Why the planning shortfall?
Well, at least in part, we have NERVTAG to thank for this too
/25
Back to 2016 & the very sexy sounding 'Sub-committee on the pandemic influenza Facemasks & Respirators stockpile'
I know. I was dumb to all this behind the scenes stuff then, too
TL/DR: FFP3 for AGPs, else FRSM; pandemic stockpile procurement adjusted accordingly
Oh dear
/26


I know. I was dumb to all this behind the scenes stuff then, too
TL/DR: FFP3 for AGPs, else FRSM; pandemic stockpile procurement adjusted accordingly
Oh dear
/26



And who signed this off?
The recently knighted but had SARS2 so couldn't attend to collect it JVT, & the present NERVTAG member & 'expert' on all things face masks & respirators, SAGE EMG member [& there hearing endless affirmation of airborne SARS2 since April 2020] Dr BK
/27
The recently knighted but had SARS2 so couldn't attend to collect it JVT, & the present NERVTAG member & 'expert' on all things face masks & respirators, SAGE EMG member [& there hearing endless affirmation of airborne SARS2 since April 2020] Dr BK
/27

I've mentioned this before elsewhere & its another one for reporting, but a PubMed search for 'Killingley B' reveals an easy to peruse list, 2 of which (from 2011/13) affirm the greater filtration protection of RPE, & reference data affirming the airborne nature of flu
/28
/28
Back to the BMA report & the statements about PPE, I hope you realise a few hard truths:
1. The NHS workforce was primed for pandemic disaster thanks to inadequate RPE stockpile, following a flawed appraisal by NERVTAG & lack of open peer review, 2016
/29
bma.org.uk/media/5644/bma…
1. The NHS workforce was primed for pandemic disaster thanks to inadequate RPE stockpile, following a flawed appraisal by NERVTAG & lack of open peer review, 2016
/29
bma.org.uk/media/5644/bma…
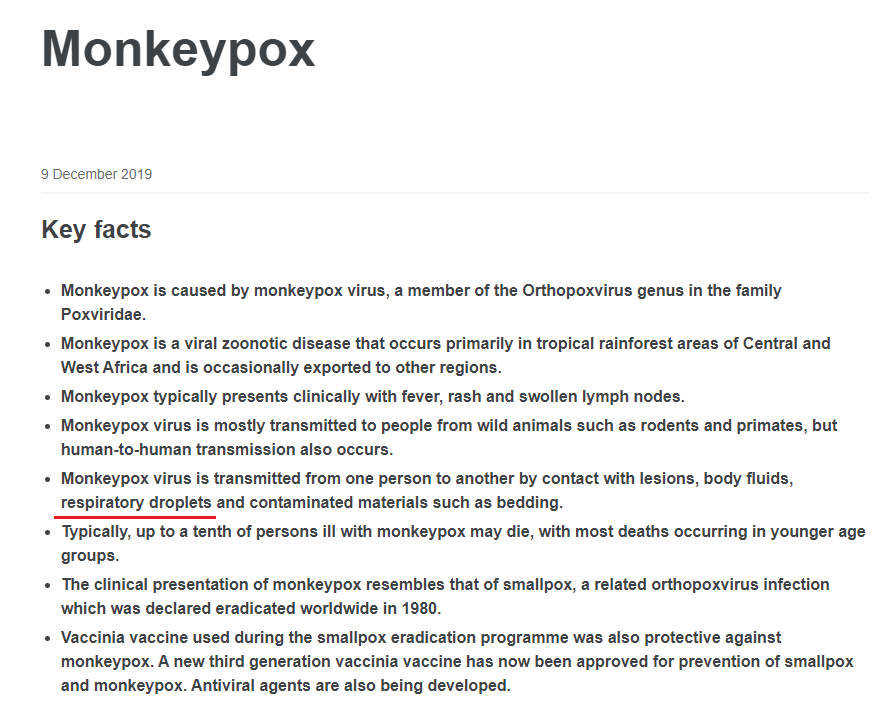
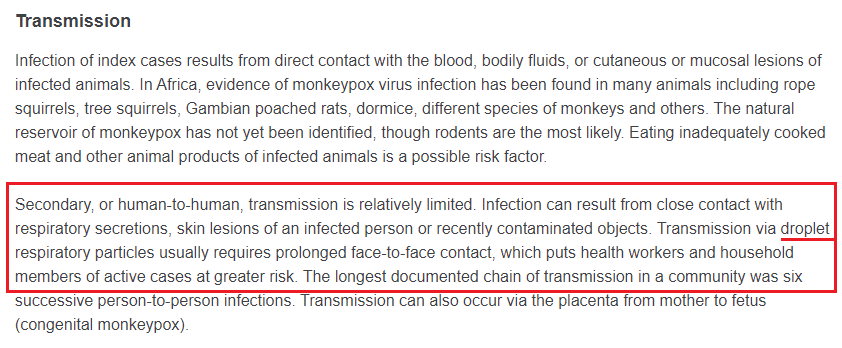
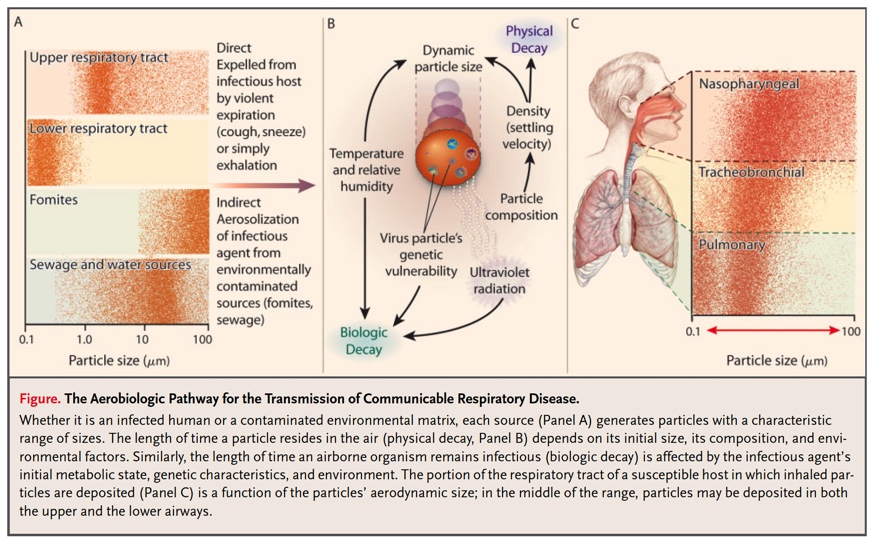
2. In Jan - early Mar 2020, SARS2 was rightly considered airborne, since its brother, SARS1 was airborne too & extensive published data known to NERVTAG members affirmed the aerosol generating capacity of normal physiological activities (coughing, speaking, breathing etc)
/30
/30
3. In early Mar 2020 the CMO alerted NERVTAG to the perilously low supplies of RPE & initiated the adaptation of pandemic RPE plans that protected those on the ICU, but left the majority of the health & social care workforce inadequately protected against SARS2 inhalation
/31
/31
4. There was no scientific data to support the IPC guidance changes
NONE
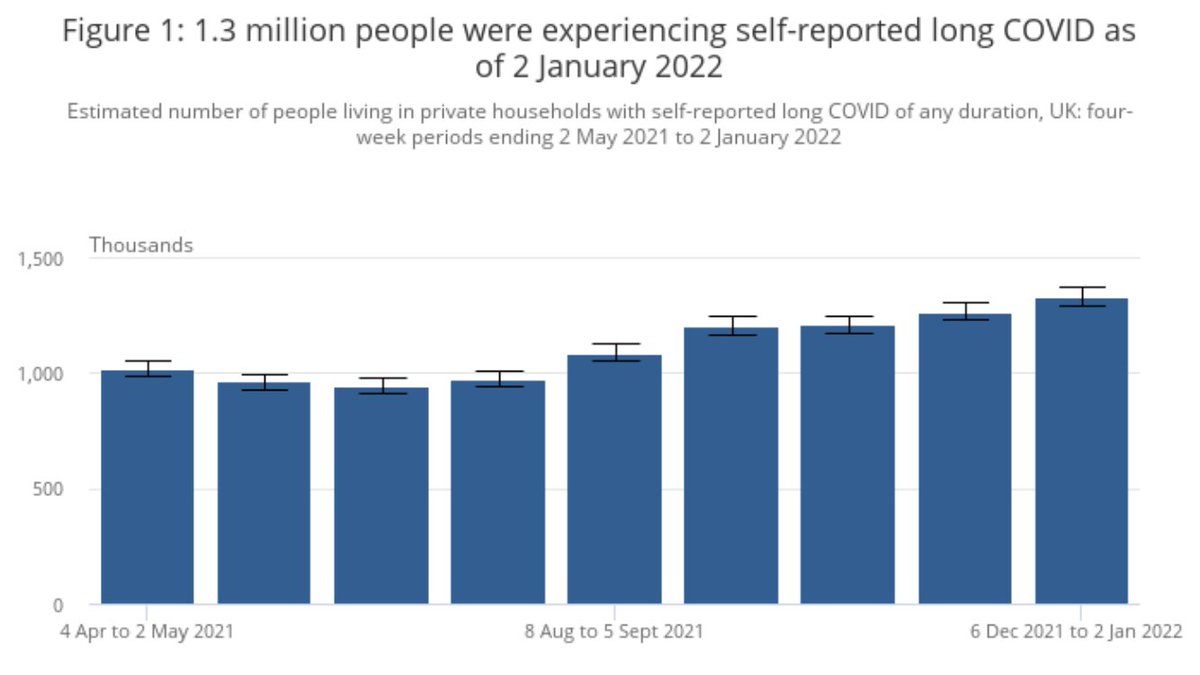
If RPE supplies were adequate, there would have been no need to revoke the airborne HCID status, the precautionary principle would have remained, & hundreds of thousands would have avoided infection
/32
NONE
If RPE supplies were adequate, there would have been no need to revoke the airborne HCID status, the precautionary principle would have remained, & hundreds of thousands would have avoided infection
/32
But more than this, by avoiding amplification of SARS2 transmission in the workplace & homes of infected HCWs, the size of the UK epidemic would have been far smaller
Even NERVTAG minutes can't avoid this truth, since nosocomial COVID19 gets a mention from April 2020...
/33
Even NERVTAG minutes can't avoid this truth, since nosocomial COVID19 gets a mention from April 2020...
/33
Now you know the qualities of our leaders
Now you know what truly motivates them
These people have received honours; they are still running the UK IPC show
Is this what is needed to 'Protect the NHS'?
End
@KamranAbbasi
bmj.com/content/372/bm…
Now you know what truly motivates them
These people have received honours; they are still running the UK IPC show
Is this what is needed to 'Protect the NHS'?
End
@KamranAbbasi
bmj.com/content/372/bm…
• • •
Missing some Tweet in this thread? You can try to
force a refresh