1/Kids now out of school? Headache already?? Usually neuroimaging doesn’t add much in headaches, but in occipital neuralgia MR neurography can add a lot.
A🧵about the use of MR neurography in occipital neuralgia
#MedTwitter #MedEd #neurorad #FOAMed #Headache #occipitalneuralgia
A🧵about the use of MR neurography in occipital neuralgia
#MedTwitter #MedEd #neurorad #FOAMed #Headache #occipitalneuralgia

2/ There are actually 3 occipital nerves:greater, lesser and least. They arise from the upper cervical nerves and innervate various areas of the dorsal scalp. The greater occipital nerve is the only one large enough to image and it arises from C2 

3/The greater occipital nerve is the largest cutaneous nerve in the body and can be traced from its origin at the dorsal ramus of C2 along the scalp in MR neurography 

4/Many pathologies can affect the greater occipital nerve, but most commonly, it is compression between muscles, resulting in occipital neuralgia. This is the basis behind Botox treatment for occipital neuralgia. Decompressive surgery can also be used to provide relief 

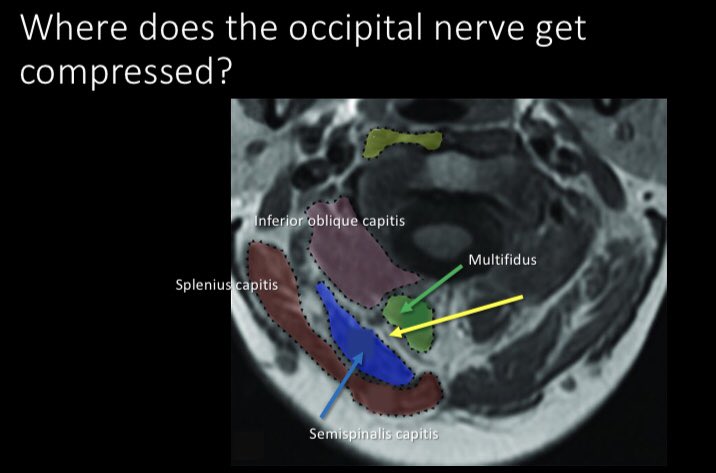
5/Where is it compressed? Usually between the multifidus and semispinalis capitis. We can use MR neurography to rule out other pathologies of the nerve and confirm compressive injury 
6/MR neurography can confirm unilateral dz preop or post op neuromas w/persistent pain. This is a pt w/unilateral right dz w/a brighter larger right nerve, indicating Sunderland 1 injury from compression
Not all headaches have to be a diagnostic headache with MR neurography 😉
Not all headaches have to be a diagnostic headache with MR neurography 😉

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















