1/ A new dx of cirrhosis…
Recurrence of cancer…
A Monday procedure is canceled & your pt waited since Friday…
We’re frequently the bearer of bad news in the hospital.
Today #MedEdTwagTeam shares tips on incorporating teaching when giving difficult news.
#MedTwitter #MedEd
Recurrence of cancer…
A Monday procedure is canceled & your pt waited since Friday…
We’re frequently the bearer of bad news in the hospital.
Today #MedEdTwagTeam shares tips on incorporating teaching when giving difficult news.
#MedTwitter #MedEd

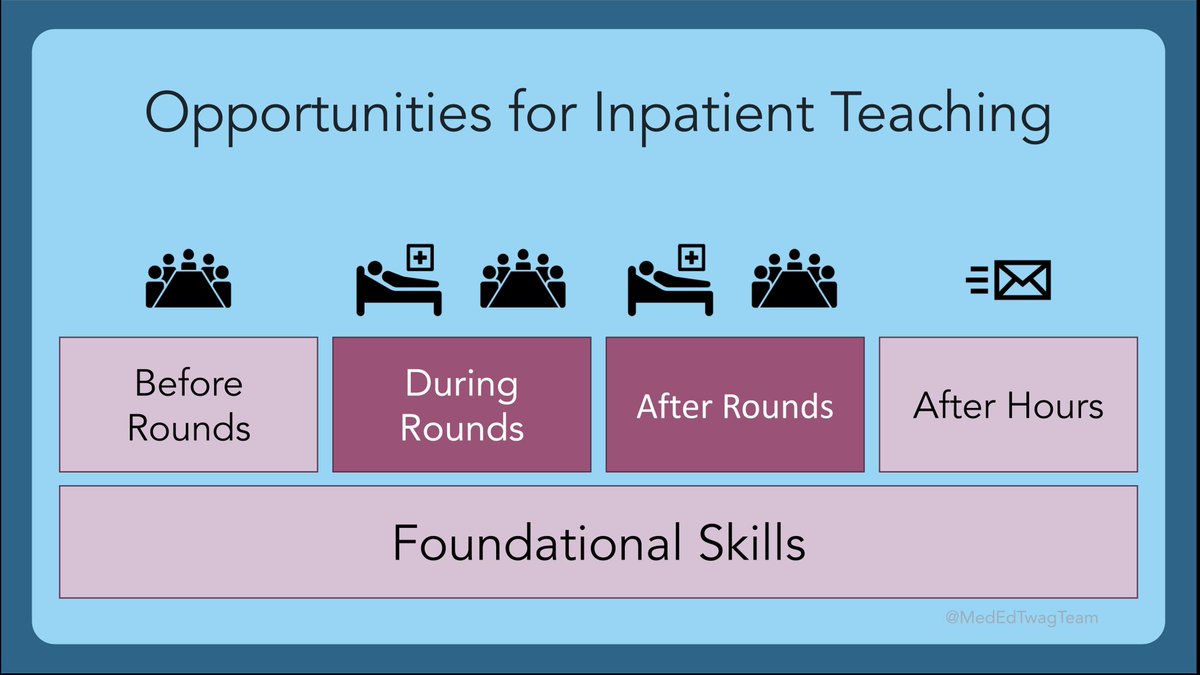
2/ As a reminder, we are continuing our discussion inpatient teaching.
Last wk, we covered tips on teaching around family meetings:
This wk, we focus on teaching when delivering difficult news, which can also be done during rounds & routine patient care
Last wk, we covered tips on teaching around family meetings:
https://twitter.com/yihanyangmd/status/1534188224314085376?s=21&t=0JQqRhk9BtAGJV7U2hnVmg
This wk, we focus on teaching when delivering difficult news, which can also be done during rounds & routine patient care
3/ But 1st… what counts as “difficult news?” We often think of cancer or terminal illnesses.
But with the definition ⬇️ I think we can agree there are plenty of times when we may be delivering difficult news to patients without even identifying it as such.
But with the definition ⬇️ I think we can agree there are plenty of times when we may be delivering difficult news to patients without even identifying it as such.

4/ At the end of last wks 🧵 on family meetings, I shared a schematic on steps before, during, and after family meetings. These same steps could be altered for delivery of difficult news.
I’d like to highlight a few updated points to this approach for delivering difficult news
I’d like to highlight a few updated points to this approach for delivering difficult news

5/ For your pre-brief: there are several frameworks available to structure the delivery of difficult news that you can review with a learner prior to news delivery.
SPIKES is one commonly-used framework developed by Braile, Buckman, et al
pubmed.ncbi.nlm.nih.gov/10964998/
SPIKES is one commonly-used framework developed by Braile, Buckman, et al
pubmed.ncbi.nlm.nih.gov/10964998/

6/ I also wanted to highlight an excellent tip brought up by @harryhan08 last week to include in your pre-brief: identify a “signal” that your learner can use to indicate that they want you to jump in and help out:
https://twitter.com/harryhan08/status/1534242088476233728?s=20&t=pVMcQkfnWYewC6RSzLafBA
7/ In addition to clear communication, delivering difficult news is the perfect time to teach / reenforce strategies that help learners develop empathic connections with patients. This is a crucial skill that can be used in any – if not ALL -- patient encounters.
8/ The @ACHonline has an excellent resource on the NURS framework for engaging empathically w/ pts. See the pocket card ⬇️ for the framework & sample phrases.
This framework is what I find myself role modeling the most during difficult news delivery.
This framework is what I find myself role modeling the most during difficult news delivery.

9/ Delivering difficult news can be tough not just for the pts, but for us as clinicians as well.
It’s important to acknowledge & normalize this, esp when your learners are delivering the news.
Make sure to NURS your team’s emotions around delivery of the news during debrief
It’s important to acknowledge & normalize this, esp when your learners are delivering the news.
Make sure to NURS your team’s emotions around delivery of the news during debrief

10/ #MedTwitter, what additional tips or strategies do you have when you are teaching learners about delivering difficult news? 

11/ Stay tuned for next week’s #TweetorialTuesday by @JenniferSpicer4 on Patient Education
Make sure to follow our other @MedEdTwagTeam members @GStetsonMD @ChrisDJacksonMD so you don’t miss anything!
Make sure to follow our other @MedEdTwagTeam members @GStetsonMD @ChrisDJacksonMD so you don’t miss anything!

• • •
Missing some Tweet in this thread? You can try to
force a refresh





















