1/Understanding cervical radiculopathy is a pain in the neck! But knowing the distributions can help your search
A 🧵to help you remember cervical radicular pain distributions #medstudenttwitter #medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #backpain #spine #Neurosurgery
A 🧵to help you remember cervical radicular pain distributions #medstudenttwitter #medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #backpain #spine #Neurosurgery

2/First, a rule of thumb—or rather a rule of elbow! You have 10 fingers. If you divide that in half, you get 5. Similarly, if you divide your arm in half at the elbow, you get 5--C5 that is! C5 radiates towards the elbow. So if it radiates below this, it is > C5 & above is < C5 

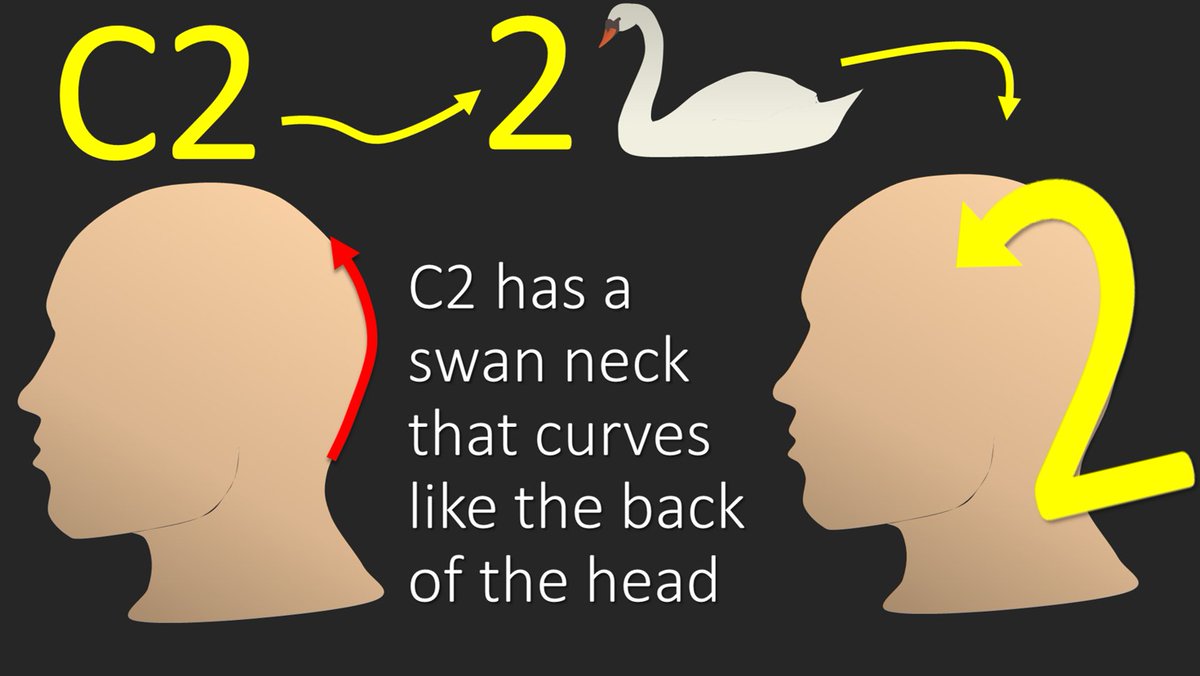
3/So let’s start with C2. C2 predominantly radiates along the dorsal aspect of the scalp, as it supplies the greater occipital nerve. I remember this bc the number 2 has a swan like neck that mimics the contour of the back of the head and its distribution 
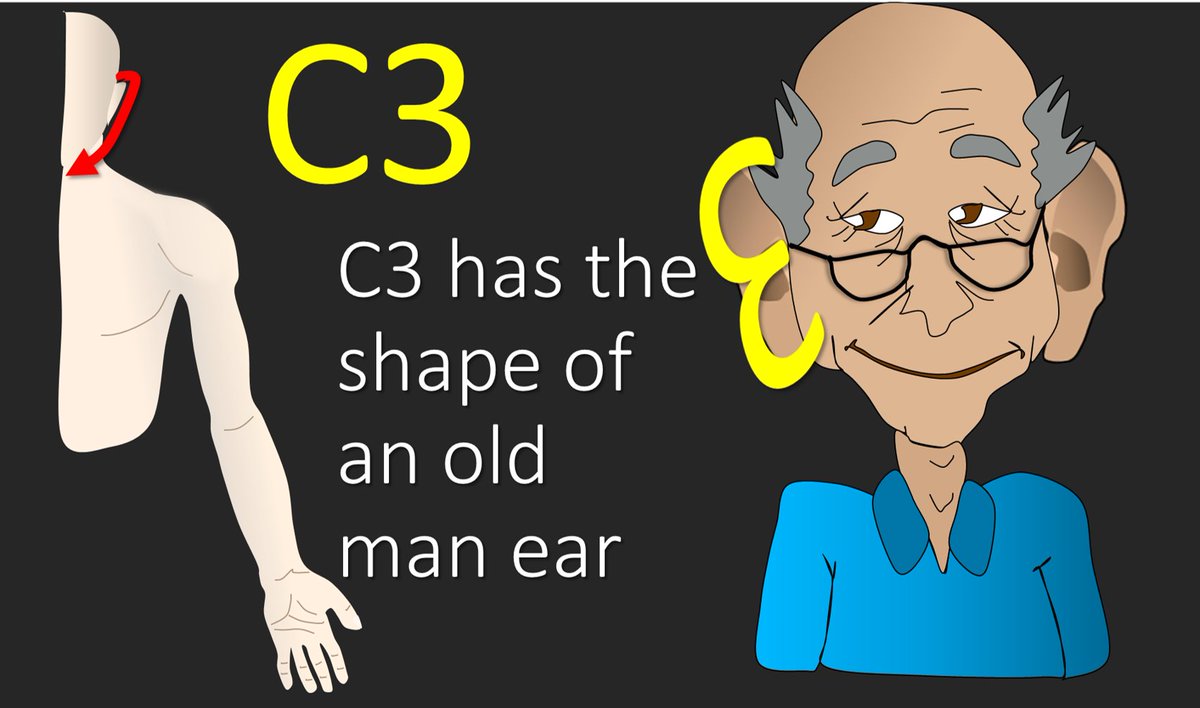
4/Next is C3. C3 starts radiating right around the ear and circles around to the front of the neck, as it is a contributor to the great auricular nerve and anterior cutaneous nerve of the neck. I remember how it starts bc the number 3 looks like those big grandpa ears. 
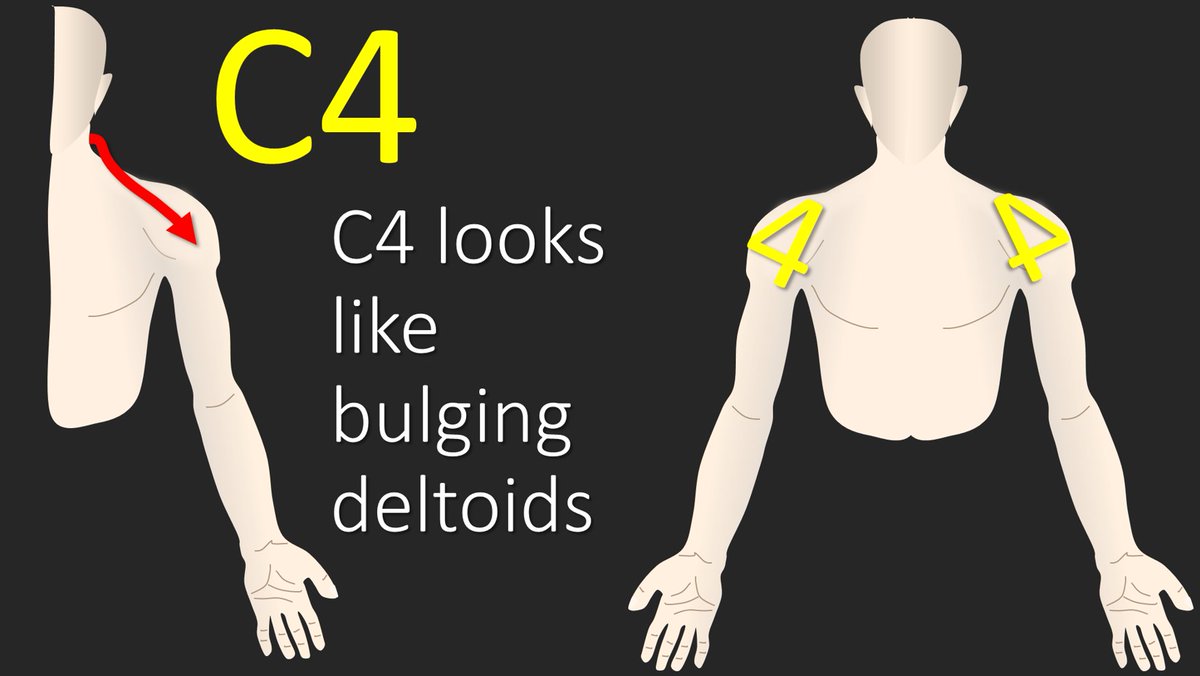
5/C4 radiates along the suprclavicular fossa, as it helps innervate the supraclavicular nerve, and goes towards the deltoid. I remember this because the triangular part of the number 4 looks the bulging deltoids that you always see on TV, but never in real life 😂 
6/I remember C5 using that general rule that half of the number of fingers (5) equals halfway down the arm (elbow). C5 radiates towards the elbow. 

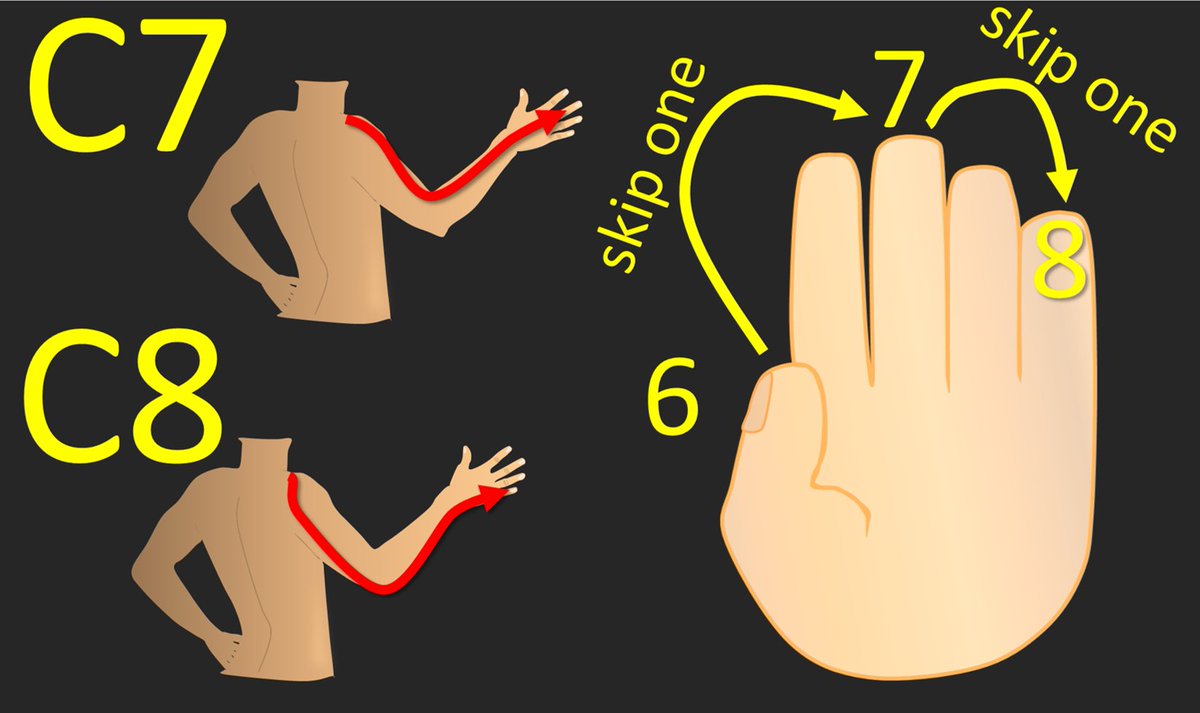
7/C6 radiates to the thumb. I remember this because when you count to 6, you use up all the fingers on one hand and then end on the thumb of the next hand. So you end on a thumb when you count to 6 and C6 radiates to the thumb 

8/We only have two cervical nerves left (C7, C8) for the 4 fingers left. So we will just use every other finger. So starting with C6 at the thumb—skip a finger gets you to the middle finger, that’s C7, skip the next finger gets you to the pinky, and that’s C8! 
9/Now you know where in the c-spine to look when a patient has pain radiating from the neck—but remember there are subtleties to this & these are general guidelines to help you. Hopefully, remembering cervical radicular pain distributions will no longer be a pain in the neck!
• • •
Missing some Tweet in this thread? You can try to
force a refresh






















