What's going on with the Impella?
As a follow up to my previous #tweetorial on the IABP, this🧵 will explore the nuts and bolts of the Impella for those in the CCU
Special thanks to @AHajduczok for helping with this🧵.
#medtwitter #cardiotwitter
As a follow up to my previous #tweetorial on the IABP, this🧵 will explore the nuts and bolts of the Impella for those in the CCU
Special thanks to @AHajduczok for helping with this🧵.
#medtwitter #cardiotwitter
@AHajduczok Learning objectives:
💔 history of the Impella
💔 learn how it works
💔 how to troubleshoot when it doesn't work
💔 history of the Impella
💔 learn how it works
💔 how to troubleshoot when it doesn't work
@AHajduczok The Impella is based on concept from Egypt in the 3rd Century BC
The Greek mathematician Archimedes, developed a machine to raise water up while in Egypt. The machine consists of a screw within a hollow cylinder that transfers water upwards by each segment of the screw.
The Greek mathematician Archimedes, developed a machine to raise water up while in Egypt. The machine consists of a screw within a hollow cylinder that transfers water upwards by each segment of the screw.
@AHajduczok Dr. Richard Wampler adapted the design in 1985 by inventing the Hemopump, the first intravascular axial flow LV support device.
In 1988, the Hemopump was successfully implanted in a patient at @Texas_Heart. However, it was never a commercial success and was soon discontinued.
In 1988, the Hemopump was successfully implanted in a patient at @Texas_Heart. However, it was never a commercial success and was soon discontinued.

@AHajduczok @Texas_Heart In 1991, Dr. Thorsten Siess modified the Hemopump to include a shorter rotor and the addition of a motor on the catheter itself.
This gave rise to the Impella class of products that were approved for clinical use in Europe (2005) and the US (2008).
ncbi.nlm.nih.gov/pmc/articles/P…
This gave rise to the Impella class of products that were approved for clinical use in Europe (2005) and the US (2008).
ncbi.nlm.nih.gov/pmc/articles/P…
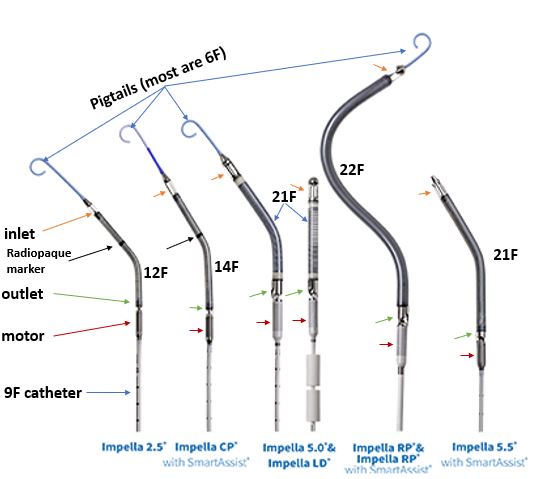
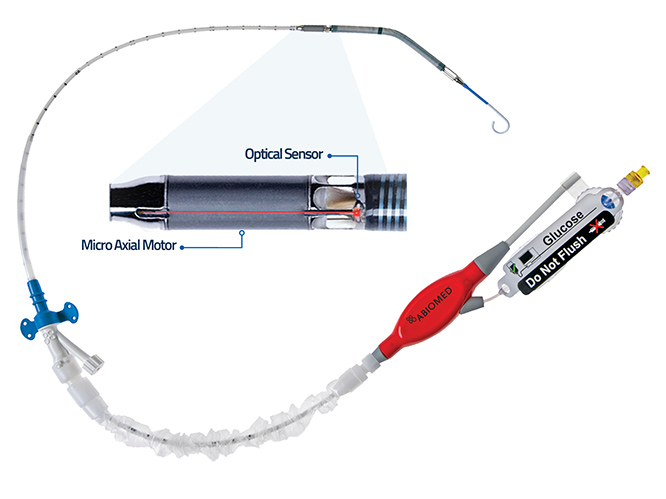
@AHajduczok @Texas_Heart What are the important components of the Impella?
Inlet: 4 (or 5) openings that draws blood into cannula
Cannula: spiral shaped body made of nitinol and polyurethane
Outlet: where blood exits cannula
Motor: powers rotor in outlet
Marker: for positioning (only on 2.5 and CP)
Inlet: 4 (or 5) openings that draws blood into cannula
Cannula: spiral shaped body made of nitinol and polyurethane
Outlet: where blood exits cannula
Motor: powers rotor in outlet
Marker: for positioning (only on 2.5 and CP)
@AHajduczok @Texas_Heart Indications include:
💔 cardiogenic shock immediately (<48 hours) following acute MI or CABG
💔 cardiogenic shock in the setting of cardiomyopathy or myocarditis
💔 during high risk PCI
💔 cardiogenic shock immediately (<48 hours) following acute MI or CABG
💔 cardiogenic shock in the setting of cardiomyopathy or myocarditis
💔 during high risk PCI
@AHajduczok @Texas_Heart Contraindications include:
🚫 LV pathology (thrombus, rupture, VSD)
🚫 Aortic valve pathology (Mod/severe AR, significant AS, mechanical aortic valve)
🚫 Significant right ❤️ failure (can also use RP for RV support)
🚫 Cardiac tamponade
🚫 Severe PAD that precludes placement
🚫 LV pathology (thrombus, rupture, VSD)
🚫 Aortic valve pathology (Mod/severe AR, significant AS, mechanical aortic valve)
🚫 Significant right ❤️ failure (can also use RP for RV support)
🚫 Cardiac tamponade
🚫 Severe PAD that precludes placement
@AHajduczok @Texas_Heart Duration of use is dependent on the model and indication:
For cardiogenic shock:
💓<4 days for Impella 2.5 and CP
💓<14 days for Impella 5.0, 5.5, LD, and RP
For high risk PCI:
💓 <6 hours for Impella 2.5 and CP
For cardiogenic shock:
💓<4 days for Impella 2.5 and CP
💓<14 days for Impella 5.0, 5.5, LD, and RP
For high risk PCI:
💓 <6 hours for Impella 2.5 and CP
@AHajduczok @Texas_Heart What's the difference between the models?
⚡ The numbers indicate the maximum hemodynamic support by the model
⚡ The later models (RP, 5.0, LD, and 5.5) all feature a differential pressure sensor
⚡ All models except for 2.5 feature Smart Assist®️
⚡ The numbers indicate the maximum hemodynamic support by the model
⚡ The later models (RP, 5.0, LD, and 5.5) all feature a differential pressure sensor
⚡ All models except for 2.5 feature Smart Assist®️
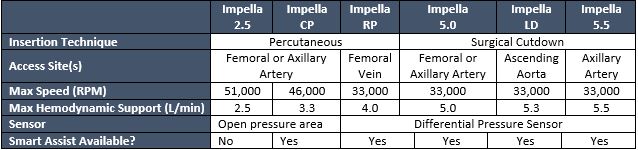
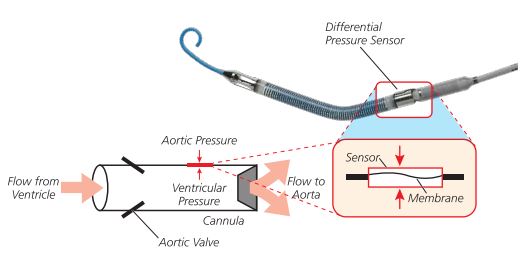
@AHajduczok @Texas_Heart What is the differential pressure sensor?
It's a membrane that flexes when there is a pressure differential between the outer surface (aortic pressure) and inner surface (ventricular pressure)
This is an important concept related to the placement signals on the monitor
It's a membrane that flexes when there is a pressure differential between the outer surface (aortic pressure) and inner surface (ventricular pressure)
This is an important concept related to the placement signals on the monitor
@AHajduczok @Texas_Heart What is Smart Assist®️ ?
It's an optical sensor that assists with catheter repositioning without image guidance
It also provides more advanced hemodynamic data such as:
⚡ LVEDP
⚡ MAP
⚡ cardiac power output (CPO) = [(MAPxCO)/451]
It's an optical sensor that assists with catheter repositioning without image guidance
It also provides more advanced hemodynamic data such as:
⚡ LVEDP
⚡ MAP
⚡ cardiac power output (CPO) = [(MAPxCO)/451]
@AHajduczok @Texas_Heart What information is found on the Impella monitor?
Placement signal: pressure differential between LV and aorta (⬆️ in diastole, ⬇️ in systole)
Motor current: a measure of load on the device (⬆️ in systole, ⬇️ in diastole)
Flow control: where you would find P-level (more next)
Placement signal: pressure differential between LV and aorta (⬆️ in diastole, ⬇️ in systole)
Motor current: a measure of load on the device (⬆️ in systole, ⬇️ in diastole)
Flow control: where you would find P-level (more next)

@AHajduczok @Texas_Heart What's up with the Performance (P) level?
It is a measure of flow that corresponds to both motor current and RPMs of the device
Factors such as improper positioning and suction events can reduce flow rates at a given P level
...but what is the right position??
It is a measure of flow that corresponds to both motor current and RPMs of the device
Factors such as improper positioning and suction events can reduce flow rates at a given P level
...but what is the right position??

@AHajduczok @Texas_Heart Using both TTE and TEE, optimal positioning includes (see 👇):
1️⃣ inlet 3.5 cm below aortic valve
2️⃣ outlet well above the aortic valve
3️⃣ catheter angled toward the LV apex
1️⃣ inlet 3.5 cm below aortic valve
2️⃣ outlet well above the aortic valve
3️⃣ catheter angled toward the LV apex
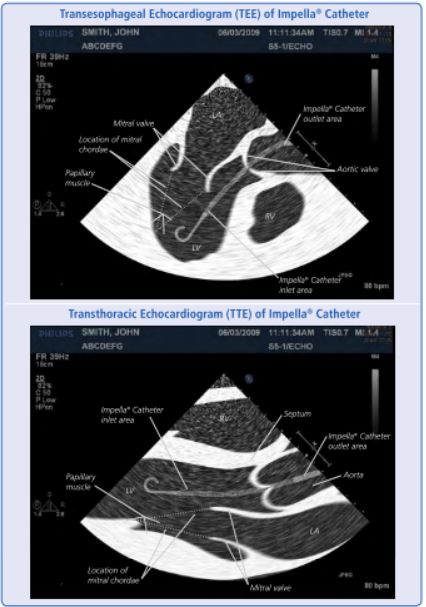
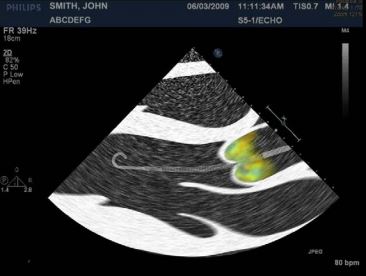
@AHajduczok @Texas_Heart Correct positioning can also be confirmed through color doppler.
If the catheter is positioned properly, you would expect turbulent flow above the aortic valve (indicating the outlet is above the valve)
If the catheter is positioned properly, you would expect turbulent flow above the aortic valve (indicating the outlet is above the valve)
@AHajduczok @Texas_Heart Now let's cover some of the common issues that can arise with the Impella
💔 improper positioning
💔 Suction alarms
💔 Hemolysis
💔 improper positioning
💔 Suction alarms
💔 Hemolysis
@AHajduczok @Texas_Heart Malpositioning can be identified by the waveforms
💔 if placed too far in the LV, you will see a ventricular waveform with a flattened motor current (A)
💔 if placed too high in aorta, you will see an aortic waveform with a flattened motor current (B)
💔 if placed too far in the LV, you will see a ventricular waveform with a flattened motor current (A)
💔 if placed too high in aorta, you will see an aortic waveform with a flattened motor current (B)
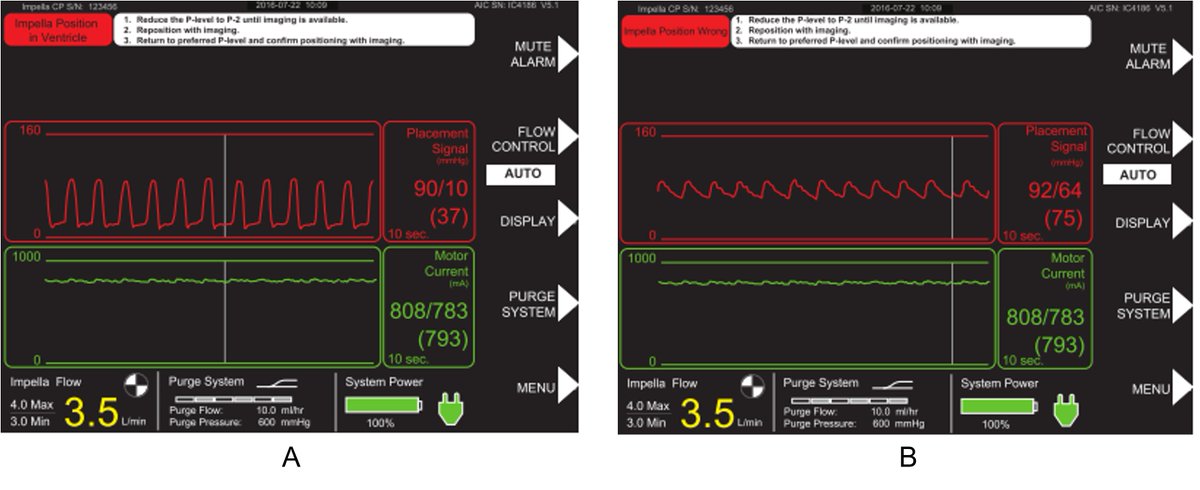
@AHajduczok @Texas_Heart How do you manage when your Impella is malpositioned?
⬇️ P level to P2 and (normally under fluoroscopic or echo guidance) slowly advance/retract the catheter until the inlet is located 3.5cm below the aortic valve annulus
THEN, slowly re-establish flow up to the desired P level
⬇️ P level to P2 and (normally under fluoroscopic or echo guidance) slowly advance/retract the catheter until the inlet is located 3.5cm below the aortic valve annulus
THEN, slowly re-establish flow up to the desired P level
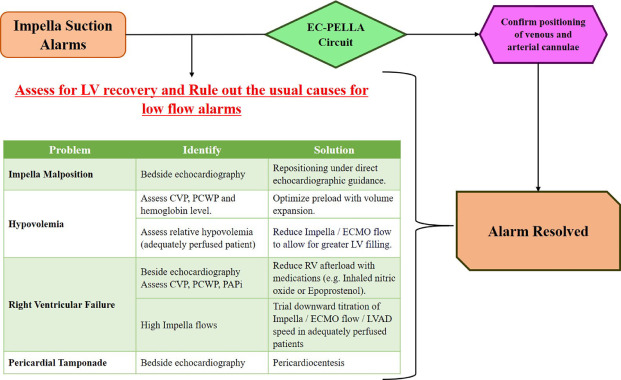
@AHajduczok @Texas_Heart Suction alarms are another issue that can arise with your Impella
Causes include:
💔 malpositioning (notice a theme here)
💔 hypovolemia
💔 RV failure
💔 Pericardial effusion → tamponade
Here's a great summary of causes and ways to correct it below: cjcopen.ca/article/S2589-…
Causes include:
💔 malpositioning (notice a theme here)
💔 hypovolemia
💔 RV failure
💔 Pericardial effusion → tamponade
Here's a great summary of causes and ways to correct it below: cjcopen.ca/article/S2589-…
@AHajduczok @Texas_Heart Hemolysis 🩸 is the final not-so-subtle complication of the Impella, but how does it happen?
🩸 when blood travels through small spaces, velocity goes ⬆️ which ⬆️ shear forces → hemolysis
🩸 hemolysis also occurs when the catheter is malpositioned due to turbulent blood flow
🩸 when blood travels through small spaces, velocity goes ⬆️ which ⬆️ shear forces → hemolysis
🩸 hemolysis also occurs when the catheter is malpositioned due to turbulent blood flow
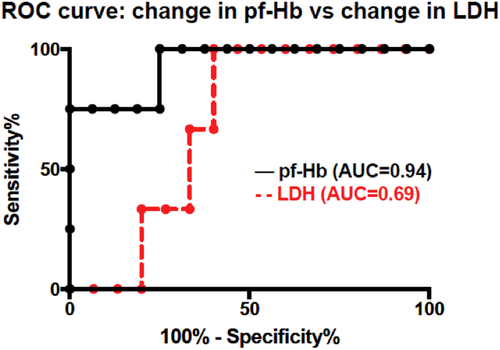
@AHajduczok @Texas_Heart How can we recognize hemolysis?
First,
🩸 look for blood in the foley (see photo 👇)
🩸 is there a new decrease in CVP and PCWP?
🩸 is the Impella in the right position?
Lab findings
⬆️ LDH, indirect bilirubin, and plasma-free hemoglobin (see graph 👇 )
⬇️ Hgb, haptoglobin

First,
🩸 look for blood in the foley (see photo 👇)
🩸 is there a new decrease in CVP and PCWP?
🩸 is the Impella in the right position?
Lab findings
⬆️ LDH, indirect bilirubin, and plasma-free hemoglobin (see graph 👇 )
⬇️ Hgb, haptoglobin

@AHajduczok @Texas_Heart Once we identify hemolysis, how can we fix it?
🩸 Correct any positioning or suction alarms
🩸 repeat labs to prove that hemolysis is occurring
🩸 give back fluid or blood if CVP or PCWP <10mmHg
🩸 Correct any positioning or suction alarms
🩸 repeat labs to prove that hemolysis is occurring
🩸 give back fluid or blood if CVP or PCWP <10mmHg
@AHajduczok @Texas_Heart Remember, do not touch the Impella if you are not familiar and trained with the device and only if and when you have approval from your attending. If you are a resident, call your fellow and/or attending immediately if these issues arise.
@AHajduczok @Texas_Heart Hopefully you found this🧵 helpful, and it will make your time in the CCU just a little bit easier!
Recommendations for further reading:
academic.oup.com/eurheartjsupp/…
pubmed.ncbi.nlm.nih.gov/35184086/
Recommendations for further reading:
academic.oup.com/eurheartjsupp/…
pubmed.ncbi.nlm.nih.gov/35184086/
• • •
Missing some Tweet in this thread? You can try to
force a refresh