1/Remembering spinal fracture classifications is back breaking work!
A #tweetorial to review the scoring system for thoracic & lumbar fractures—“TLICS” to the cool kids! #medstudenttwitter #medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #backpain #spine #Neurosurgery
A #tweetorial to review the scoring system for thoracic & lumbar fractures—“TLICS” to the cool kids! #medstudenttwitter #medtwitter #radres #FOAMed #FOAMrad #neurorad #Meded #backpain #spine #Neurosurgery

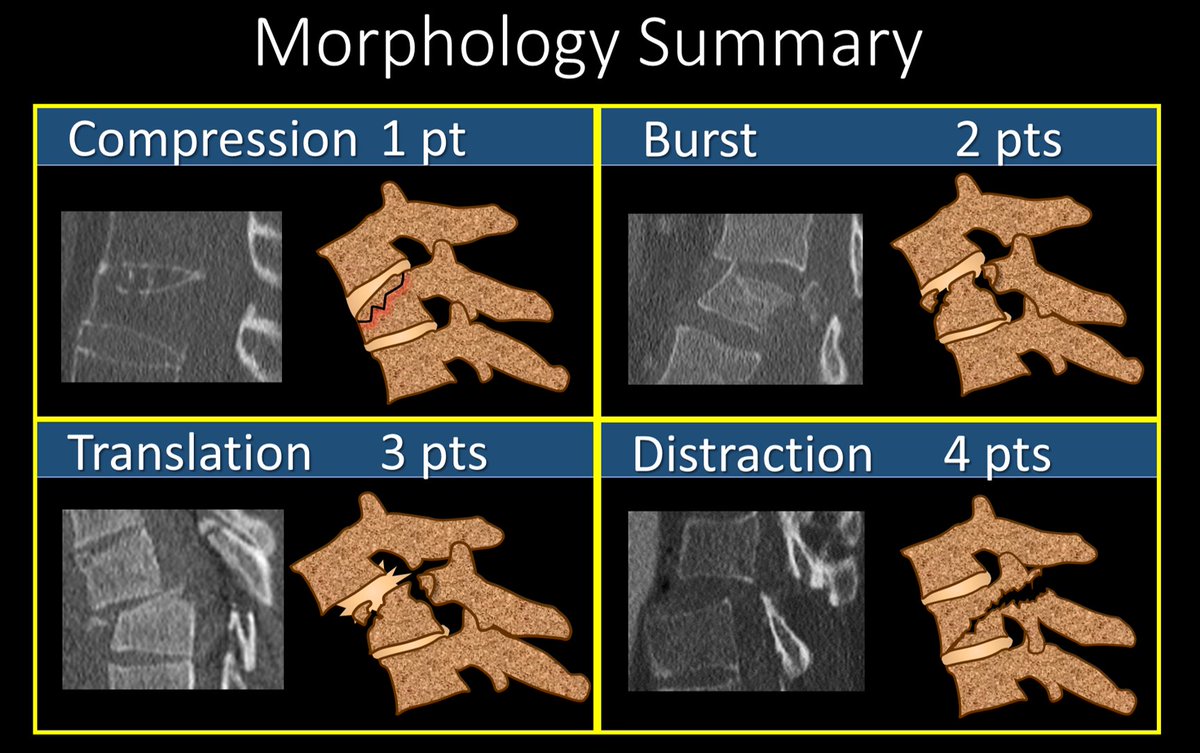
2/We’ll talk about the imaging part of TLICS. TLICS scores a fx on (1) morphology & (2) posterior ligamentous complex (PLC) injury. Let’s start w/morphology. W/only mild axial loading, you get the simplest fx, a compression fx—like a simple long bone fx--worth 1 pt. 

3/As the axial force grows, this becomes a burst fx with retropulsion of the posterior vertebral body—just as greater force causes more comminution in long bone fxs. A burst is worth 2 points. 

4/If the force is shearing, rather simply compress a vertebral body, you rip the connection between the vertebral bodies—this is the equivalent of pulling on a long bone & causing its dislocation from its joint or connection with another bone. This is worth 3 points 

5/Similar to shear forces, distracting forces will rip the vertebral bodies apart. But rather than sliding forward or back, the vertebral bodies are pulled up or down, resulting in a vertical gap between the vertebral bodies. This is worth 4 points 

6/This summarizes the TLICS scoring for fracture morphology. The higher the number, the greater the force and injury to the spine—ranging from simple compression fxs worth only 1 point to where the spine is literally ripped apart—a distraction injury, worth 4 points. 
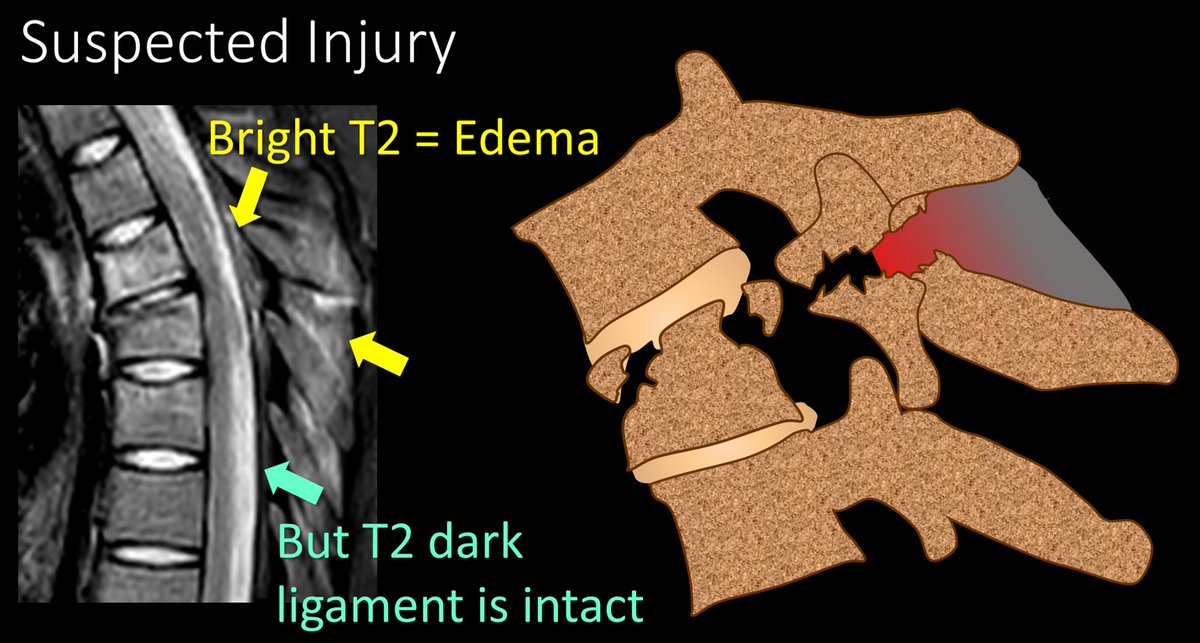
7/The next TLICS imaging finding is the integrity of the PLC. If it is intact, you get 0 pts. If you needed a tweetorial for that, well…I can’t help you much. If there is edema, but no true rupture on MRI, that is worth 2 pts. True disruption on MRI is worth 3 pts. 

8/Here is an example of suspected injury—edema is seen in the posterior ligamentous complex, but the T2 dark lines that are the ligaments themselves appear intact. This is worth 2 pts. 
9/If you can find a true disruption or gap in the T2 dark line of the ligament, that is considered truly disrupted and worth 3 points. 
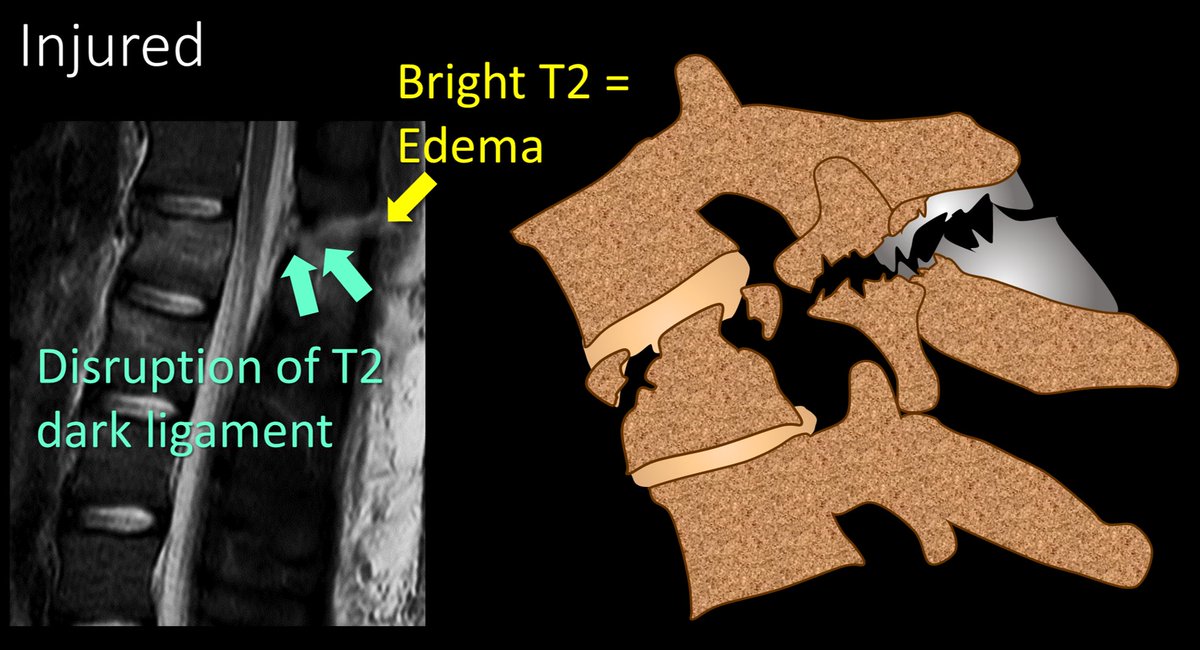
10/Here is the summary of the scoring for PLC injury in TLICS. Edema is suspicious, but only a true gap is considered injured.
So now you know how to score imaging findings in thoracolumbar fxs--I hope that takes a load off your back!
So now you know how to score imaging findings in thoracolumbar fxs--I hope that takes a load off your back!

• • •
Missing some Tweet in this thread? You can try to
force a refresh






















