1/ “When you have time, can we look over one of my notes?”
Do you have an approach to teaching when learners ask for feedback on documentation? Check out the following thread for some high-yield tips!
#MedEd #MedEdTwagTeam #TweetorialTuesday #MedTwitter
Do you have an approach to teaching when learners ask for feedback on documentation? Check out the following thread for some high-yield tips!
#MedEd #MedEdTwagTeam #TweetorialTuesday #MedTwitter

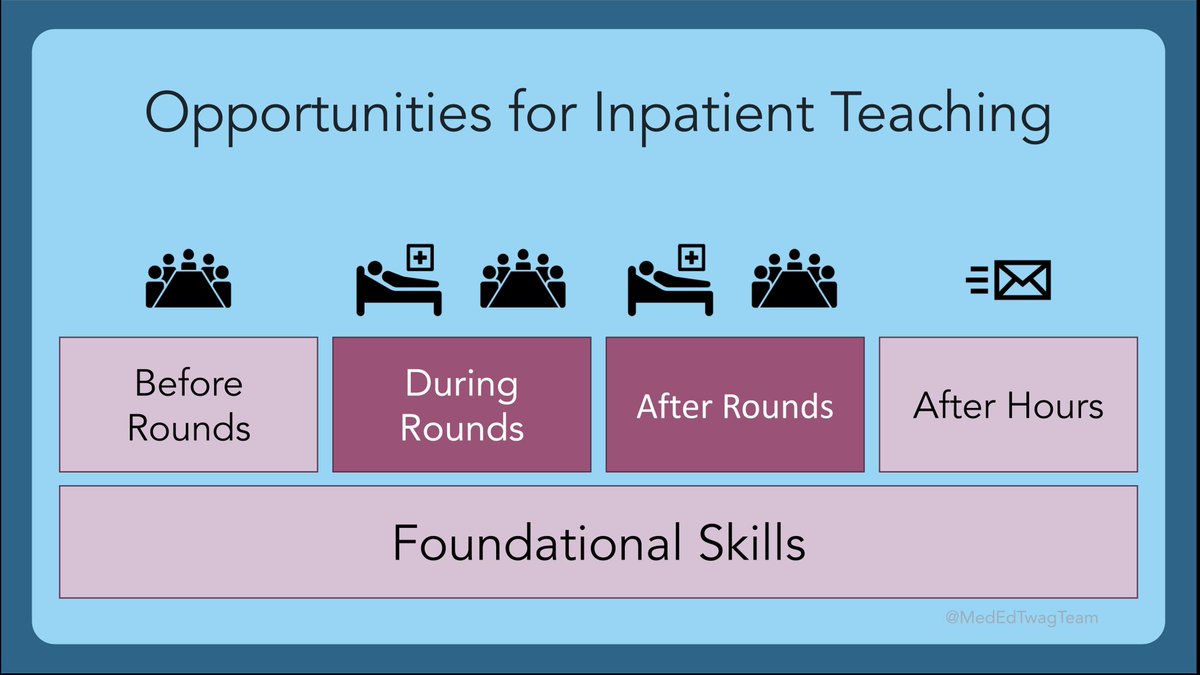
2/ As a reminder, we are still in our series on inpatient teaching. I typically will teach about notes after rounds. 

3/ First… in your opinion, how valuable is it for learners to receive feedback from notes?
#MedEd #MedTwitter #MedStudentTwitter
#MedEd #MedTwitter #MedStudentTwitter
4/ Prior studies like the 1 ⬇️ show that trainees spend majority of their days documenting in the electronic health record. Most of the time they don’t receive feedback on this documentation
jamanetwork.com/journals/jamai…
jamanetwork.com/journals/jamai…
5/ A framework for teaching with notes is below. You may recognize this framework as similar to the GO Ask-Tell-Ask model for feedback
We will focus on purpose-specific teaching in the next few tweets.
We will focus on purpose-specific teaching in the next few tweets.

6/ Purpose: Admittedly, many aspects of note-writing differ due to personal preference/style. However, there are 4 universal purposes for notes around which you can structure your teaching.
I will 1st ask my learners, “What is the purpose of us writing this note?”
I will 1st ask my learners, “What is the purpose of us writing this note?”

7/ Depending on interest & level of my learner, I choose to focus on 1 or 2 of these note purposes. Early learners tend to prefer discussing communicating w/ notes & clinical reasoning; I save discussions around billing & legal practicalities for advanced learners 

8/ Communication: Do your learners’ notes accurately and concisely communicate what is going on with the pt? Below are a few questions to consider when giving feedback on notes with a focus on communication. 

9/ Clinical Reasoning: When reviewing notes for clinical reasoning, I ask myself:
If someone unfamiliar with the pt read this note, could they understand...
❓WHAT is going on with the pt
❓WHY were these specific diagnoses, tests, & interventions chosen?
If someone unfamiliar with the pt read this note, could they understand...
❓WHAT is going on with the pt
❓WHY were these specific diagnoses, tests, & interventions chosen?
10/ Clinical Reasoning: Chart-stimulated recall (CSR) is a useful tool to further explore learners’ clinical reasoning based on a case using notes.
The following checklist by the ACGME provides sample ?s that can be used for CSR: acgme.org/globalassets/4…
The following checklist by the ACGME provides sample ?s that can be used for CSR: acgme.org/globalassets/4…

11/ For learners close to independent practice, I use notes to teach the "business" aspects of charting.
I acknowledge that billing & medical/legal purposes of notes is a byproduct of US healthcare & shouldn’t be the primary driver for what is documented in notes.
I acknowledge that billing & medical/legal purposes of notes is a byproduct of US healthcare & shouldn’t be the primary driver for what is documented in notes.

12/ SHOWING is better than TELLING. An attestation beyond “I saw & discussed the pt & agree with note” is a great way to role model examples of problem representation, concise clinical course summary, discussing complex differential diagnosis/management decisions
13/ Educators: Have you reviewed patient notes with your learners?
Learners: Have you reviewed notes with your attendings/residents?
What have you found helpful?
#MedTwitter #MedStudentTwitter #MedEd
Learners: Have you reviewed notes with your attendings/residents?
What have you found helpful?
#MedTwitter #MedStudentTwitter #MedEd

14/ Join us again next Tuesday when @ChrisDJacksonMD drops some tips on teaching after hours!
And don't forget to follow @JenniferSpicer4 @GStetsonMD @MedEdTwagTeam to ensure you don't miss a thread!
And don't forget to follow @JenniferSpicer4 @GStetsonMD @MedEdTwagTeam to ensure you don't miss a thread!

• • •
Missing some Tweet in this thread? You can try to
force a refresh