‼️ NEW Paper ‼️
In @JAMANetworkOpen, we found that VA patients with #AFib who experience homelessness had a 21% ⬇️ odds of receiving stroke-preventing anticoagulation (blood thinners).
Here's more on our journey to this #Pharmacoequity paper.
Link: ja.ma/3ODXdss
1/
In @JAMANetworkOpen, we found that VA patients with #AFib who experience homelessness had a 21% ⬇️ odds of receiving stroke-preventing anticoagulation (blood thinners).
Here's more on our journey to this #Pharmacoequity paper.
Link: ja.ma/3ODXdss
1/

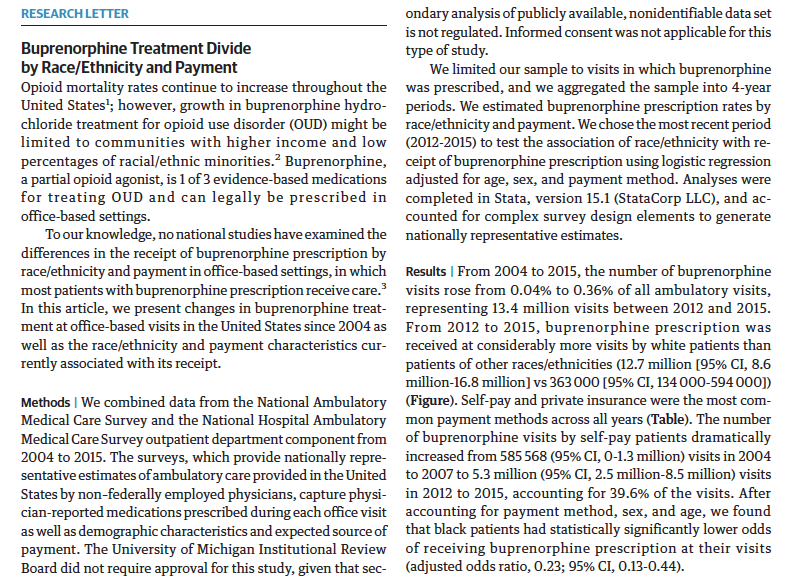
Previously, if you looked up "homeless & atrial fibrillation" in PubMed, only 5 results came up.
This included a 2003 @JAMAInternalMed study that saw that Ohio Medicaid enrollees had ⬇️ use of warfarin if they had homelessness or inadequate housing.
ja.ma/3PFwj52
2/

This included a 2003 @JAMAInternalMed study that saw that Ohio Medicaid enrollees had ⬇️ use of warfarin if they had homelessness or inadequate housing.
ja.ma/3PFwj52
2/


We started digging into this in 2019, when 1st author, David Wilson, a PittMed student & Veteran, met with me for a summer research project.
We decided to use our national #AFib cohort to see if there was a relation b/w homelessness & AF treatment.
ja.ma/3ODXdss
3/
We decided to use our national #AFib cohort to see if there was a relation b/w homelessness & AF treatment.
ja.ma/3ODXdss
3/

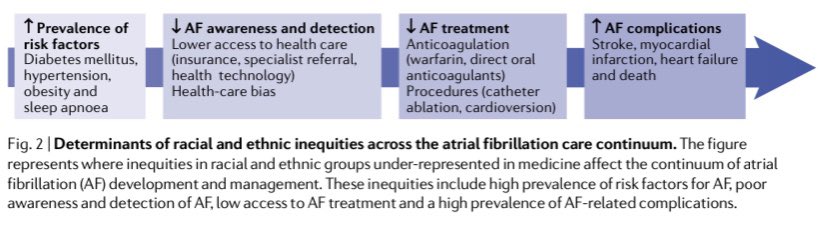
First, who were these patients? In a cohort of 164K Veterans with #AFib from 2014-20, 6,362 experienced homelessness.
We saw that Black patients (typically underrepresented in #AFib studies) were hugely overrepresented among those with homelessness.
ja.ma/3ODXdss
4/
We saw that Black patients (typically underrepresented in #AFib studies) were hugely overrepresented among those with homelessness.
ja.ma/3ODXdss
4/

Second, our top-line finding was that even when controlling for sociodemographic (age, race, disability status), clinical comorbidities, and clinician/facility factors, patients experiencing homelessness were ⬇️ likely to receive any anticoagulant 💊.
ja.ma/3ODXdss
5/
ja.ma/3ODXdss
5/
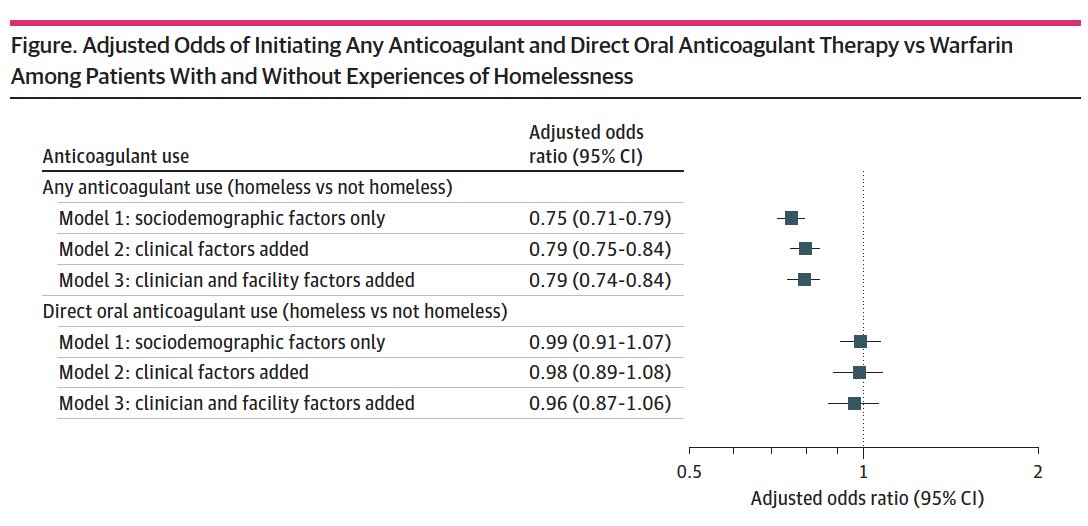
On a positive note for #Pharmacoequity in the VA, we did find that if you are started on anticoagulant therapy, there was no difference in receipt of newer DOAC medications between those experiencing homelessness and those who were not.
ja.ma/3ODXdss
6/
ja.ma/3ODXdss
6/
Third, the implications of this study are many.
In particular, how do we weigh clinical & social risk factors for patients when offering guideline-based therapies, not just for #AFib, but for the myriad conditions seen in patients w. homelessness?
ja.ma/3ODXdss
7/
In particular, how do we weigh clinical & social risk factors for patients when offering guideline-based therapies, not just for #AFib, but for the myriad conditions seen in patients w. homelessness?
ja.ma/3ODXdss
7/

I could go on but I'll end with gratitude to a 🌟🌟research team, including a med student and resident mentee and collaboration with @DrAudreyJones, whose @vahsrd Career Development Award is focused on improving mental health in homeless Veterans. 👇🏾
hsrd.research.va.gov/research/abstr…
8/
hsrd.research.va.gov/research/abstr…
8/

Also grateful to my mentors who provided their wisdom on the way to my 1st senior author original research pub... even to the point of coming off of the author list to help meet publication requirements. 🙏🏾
cc @walidgellad @jared_w_magnani @CBGood23
ja.ma/3ODXdss
9/
cc @walidgellad @jared_w_magnani @CBGood23
ja.ma/3ODXdss
9/

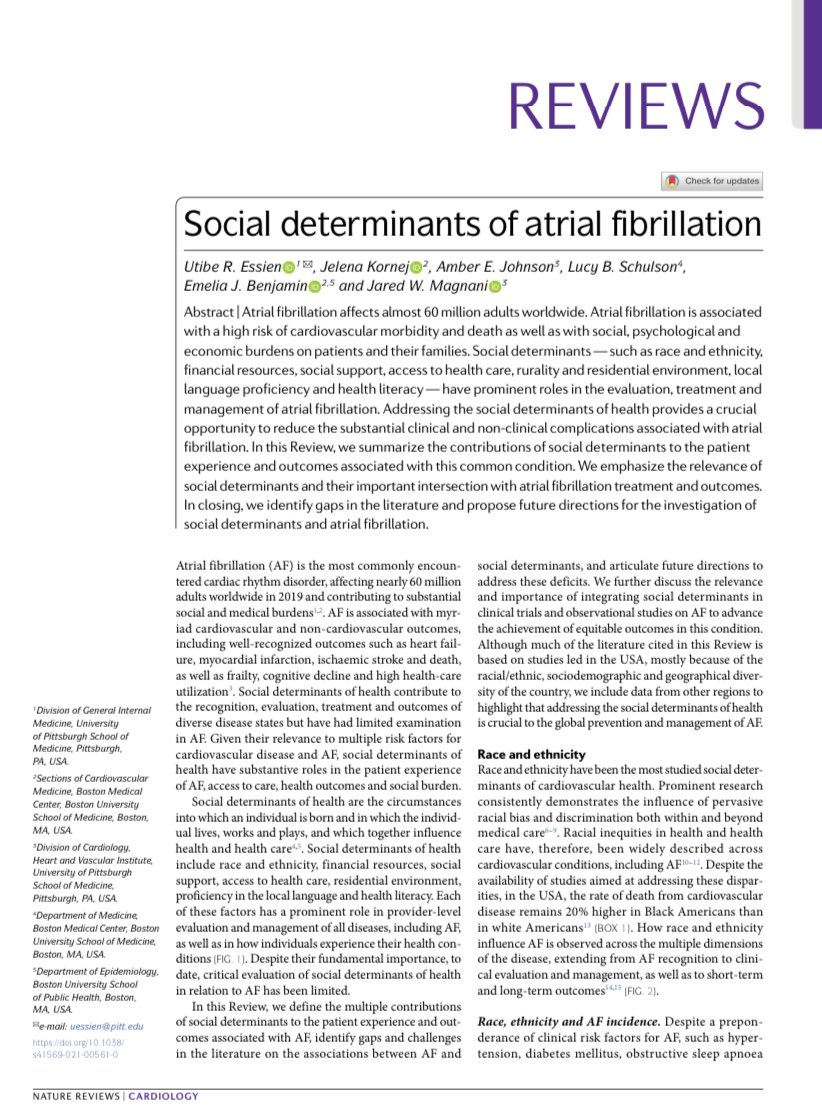
This was Paper 3 from our REACH-AF cohort, exploring #Pharmacoequity and the social determinants of #AFib.
Paper 1: 👇🏾👇🏾
Paper 2: ahajournals.org/doi/10.1161/CI…
Paper 3: ja.ma/3ODXdss
More to come. As they like to say, follow this space! 😃
10/10
Paper 1: 👇🏾👇🏾
Paper 2: ahajournals.org/doi/10.1161/CI…
Paper 3: ja.ma/3ODXdss
More to come. As they like to say, follow this space! 😃
https://twitter.com/UREssien/status/1420405793040465928?s=20&t=hx8PMBcPI5HETZZTlivrUQ
10/10
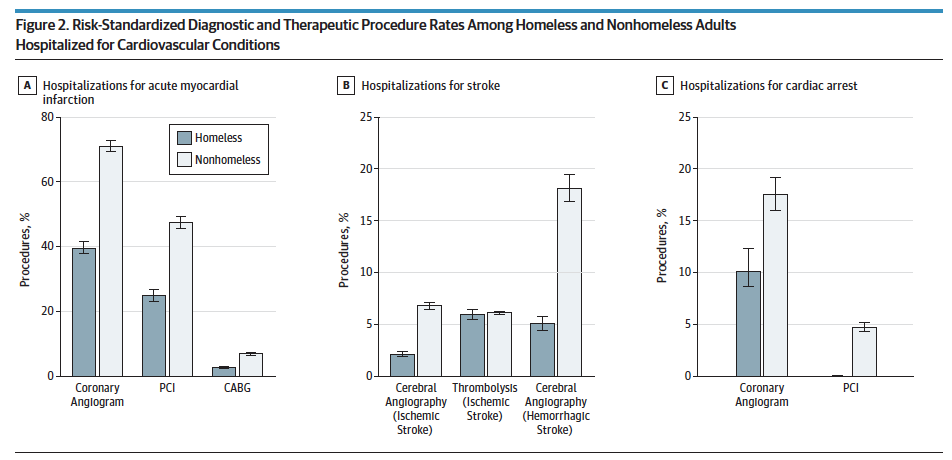
P.S. While homelessness & #AFib has been understudied, there has been important work in cardiovascular disease in general, including this study from @rkwadhera @kejoynt & team in JAMA IM.
This is a paper I reference regularly, a must-read if you haven't.
jamanetwork.com/journals/jamai…
This is a paper I reference regularly, a must-read if you haven't.
jamanetwork.com/journals/jamai…
P.P.S. To be sure, housing & health extends far beyond patients with #AFib getting blood thinners.
We’ve talked about this a lot on our #AntiracisminMedicins podcast, from the impact of redlining to the role of green spaces in health.
Take a listen. 👇🏾
clinicalproblemsolving.com/antiracism-in-…


We’ve talked about this a lot on our #AntiracisminMedicins podcast, from the impact of redlining to the role of green spaces in health.
Take a listen. 👇🏾
clinicalproblemsolving.com/antiracism-in-…



• • •
Missing some Tweet in this thread? You can try to
force a refresh