Great thread on the link of Ehlers Danlos Syndrome (EDS) and Dysautonomia/POTS.
To extend on the observations some additional points 🧵:
#1 EDS is commonly associated with venous abnormalities such as nutcracker physiology of abdominal vessels or May Thurner syndrome.

To extend on the observations some additional points 🧵:
#1 EDS is commonly associated with venous abnormalities such as nutcracker physiology of abdominal vessels or May Thurner syndrome.
https://twitter.com/AndrewCAhn2/status/1552715513859436544

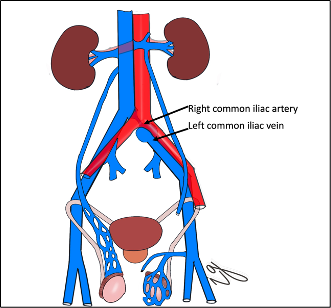
#2 The issue with venous distension in the abdomen and pelvis is that it creates venous pooling/obstruction to blood return. Its mostly in the abdomen and not legs! 





#3 The consequence are abdominal symptoms often reported by EDS and dysautonomia/POTS patients such as Chronic abdominal pain, Bladder fullness, Flank pain etc...
The Clinical Problem of Pelvic Venous Disorders
interventional.theclinics.com/article/S2211-…
The Clinical Problem of Pelvic Venous Disorders
interventional.theclinics.com/article/S2211-…

#4 Venous pooling in the abdomen and pelvis, however also leads to so called "#CardioVenous Syndrome" also known as "#Preload-Reserve-Failure".
Extracardiac Abnormalities of Preload Reserve ahajournals.org/doi/10.1161/CI…
Extracardiac Abnormalities of Preload Reserve ahajournals.org/doi/10.1161/CI…

#5 The inability to fill the heart (preload) with blood when upright ▶️ heart "runs empty". This diminishes the amount of blood being ejected from the heart. The likely consequence:
- Chronic fatigue
- Shortness of breath
- Foggy brain sensation
- Chest pain
- Migranes
...
- Chronic fatigue
- Shortness of breath
- Foggy brain sensation
- Chest pain
- Migranes
...
#6 A lot more investigations into these syndromes are needed. Greatly under-appreciated, under-tested and often mis-diagnosed. The right tests matter and more attention to the "dysautonomia" space is needed!
@Dysautonomia @manesh_patelMD @camfrazmills
ahajournals.org/doi/10.1161/CI…
@Dysautonomia @manesh_patelMD @camfrazmills
ahajournals.org/doi/10.1161/CI…
#7 How long-COVID is related to the above syndromes is unclear but significant overlap in the presentation and clinical findings exists.
Autonomic dysfunction in 018long COVID019: rationale, physiology and management strategies ncbi.nlm.nih.gov/pmc/articles/P…
Autonomic dysfunction in 018long COVID019: rationale, physiology and management strategies ncbi.nlm.nih.gov/pmc/articles/P…
#8 What we do know is that to date we have many new cases of cardiovascular disease and heart failure specifically being diagnosed post-COVID hospitalization and disentangling the physiology will takes us years!
nature.com/articles/s4146…
#End
nature.com/articles/s4146…
#End

• • •
Missing some Tweet in this thread? You can try to
force a refresh


















