ICU POCUS snippets: A bit of context: An elderly patient with hx of DM2 / HTN / HLD / peripheral vascular disease / ureteral stent & recurrent UTIs is admitted to the hospitalists’ service w diffuse abdominal pain, nausea & vomiting. Treated for a few days w antibiotics...
...but never really felt any better (weak/abd pain). Eventually, became hypotensive & was transferred to the ICU for “initiation of vasopressors”. Phys exam: diffuse abd tenderness. Formal echo earlier that day: "Normal LV/RV in size and systolic function". ICU POCUS was done...
...to gain more information regarding the cause of the abd pain and the hemodynamic picture. Some of the clips are shown here:
What is this 👆?
This is actually the pulmonary artery bifurcation. Sometimes u can even see a saddle pulmonary embolus sitting there... We usually get this view from the parasternal short axis at the AoV level aiming a bit higher. Here we were lucky to get it from a poor parasternal long axis:
It is not always as clear as in this case but, if it is, you can interrogate w color Doppler and PW/CW separately each one of the PA branches (R - L):
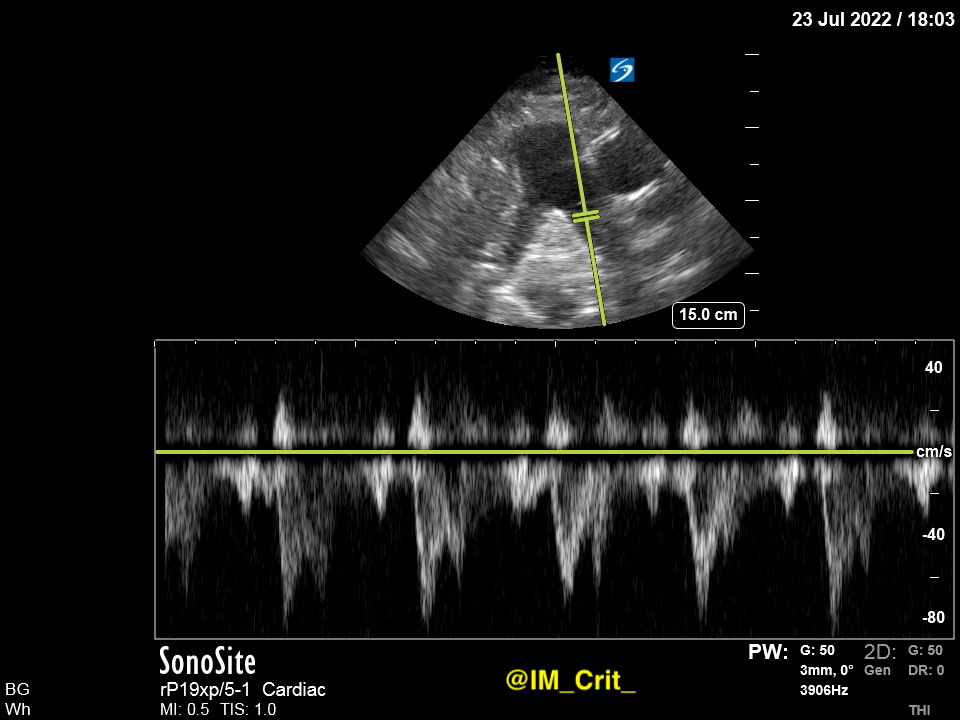
PW Doppler in one side:
How is this 👆Doppler profile of the PA artery called? @khaycock2 has a great talk on this
Yes, I know, you are wondering how all these clips changed patient's management. They didn't, mainly because a "goals of care" discussion shifted the focus of our efforts. Next time they will. And, wouldn't it be nice to make our practice less boring?
Thanks for reading!
Thanks for reading!
#POCUS #ECHOFIRST #POCUSpeeps #FOAMed #FOAMus #FOAMcc #IMPOCUS #MedTwitter #MedEd #EMBound @ACEP_EUS @MetroHealth_EM @MH_EMultrasound @jminardi21 @ThinkingCC @RJonesSonoEM @jaffa_md @katiewiskar @kyliebaker888 @TomJelic @msiuba @siddharth_dugar @thepocusatlas @iceman_ex
@NephroP @HeyDrNik @ICUltrasonica @NickjohnsonMD @EmergenxyPhysic @DraHuerta09 @pocusmeded @POCUSClub @thepocusatlas @AmbrizMau @ecocritic_es @TaotePOCUS @pocusfoamed @interconsulta @cianmcdermott @ImagenCardiaca @apenarEM @PorrosE @chileanestesia @vaszochios @nickmmark
@cjosephy @pdsalinas @GUH_ICU_Anaesth @KalagaraHari @UAlberta_Sono @EMUGs_ @UAlberta_ICU @UAB_Sono @MonaresTI @EMUGs_ @MedCriticaMex @critconcepts @pablitorf @MediCasos @ultra2ente @ACEP_EUS @grepmeded @RosenelliEM @FisioPocus @RogerAlvarezDO @MegriMohammed @emily_fri
• • •
Missing some Tweet in this thread? You can try to
force a refresh