1/ Do you prescribe Incentive Spirometry (IS) for postoperative patients?
Is the routine use of IS to prevent postoperative pulmonary complications (PPCs) a "Thing We Do For No Reason?"
Let's explore IS in the following #tweetorial!
#MedTwitter
Is the routine use of IS to prevent postoperative pulmonary complications (PPCs) a "Thing We Do For No Reason?"
Let's explore IS in the following #tweetorial!
#MedTwitter

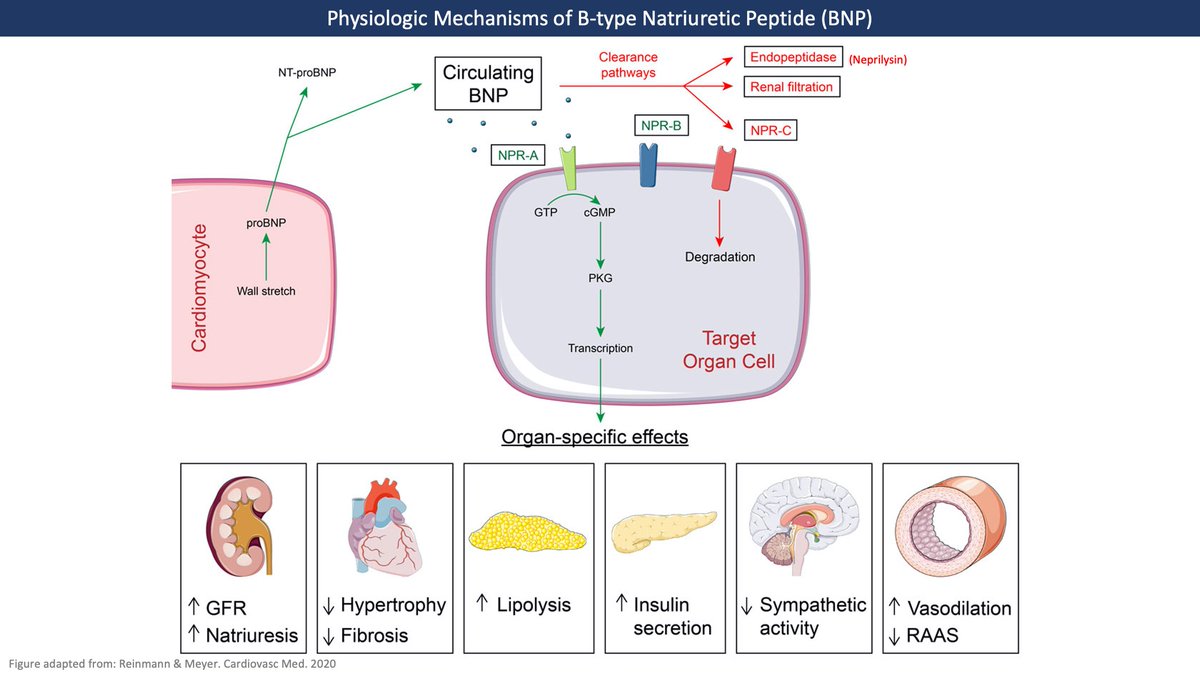
2/ PPCs are extremely common and associated with a high rate of morbidity and mortality following surgery.
While no one agrees on which conditions we should include in PPCs, most agree that atelectasis (collapsed lung tissue) is the most common PPC.
While no one agrees on which conditions we should include in PPCs, most agree that atelectasis (collapsed lung tissue) is the most common PPC.

3/ Though it's common, the significance of postoperative atelectasis isn't always clear.
While there is no evidence to support the dogma that atelectasis causes early postoperative fever, atelectasis frequently accompanies more serious complications including pneumonia & death.
While there is no evidence to support the dogma that atelectasis causes early postoperative fever, atelectasis frequently accompanies more serious complications including pneumonia & death.

4/ As early as the 1920s doctors debated the pathophysiologic causes of postoperative atelectasis and even whether mild cases were "normal".
The uncertainty of the significance of atelectasis triggered even more debate about best to treat it.
The uncertainty of the significance of atelectasis triggered even more debate about best to treat it.
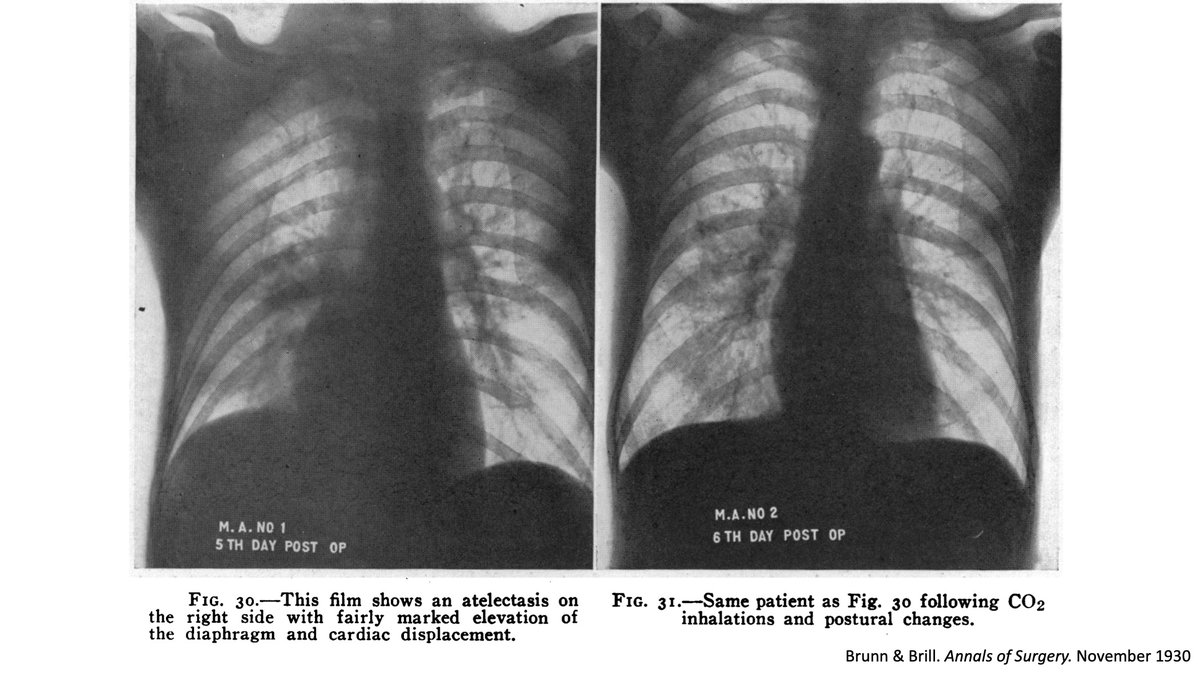
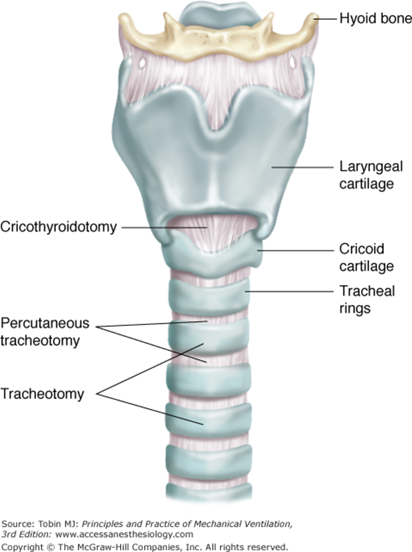
5/ Postoperative atelectasis inspired many creative treatments to re-inflate the lung including bronchoscopic aspiration, cocainization of the airway, and CO2 inhalation.
One doctor even promoted direct tracheal injections to stimulate coughing and reduce collapse.
One doctor even promoted direct tracheal injections to stimulate coughing and reduce collapse.
6/ Early on doctors recognized the importance of positional changes and deep breathing exercises in reducing atelectasis. They soon developed devices to assist patients with deep breaths including blow bottles and intermittent positive pressure breathing (IPPB) machines. 
7/ In the 1970s Bartlett introduced the incentive spirometer as a means to reverse atelectasis via alveolar recruitment. When compared with IPPB (the standard of the day), IS improved atelectasis in patients undergoing cardiac surgery.
IS soon spread rapidly!
IS soon spread rapidly!

8/ Despite widespread adoption and 50 years of use, however, there is little data to support the use IS over other methods for preventing PPCs. There is also no agreement about the best frequency, duration, and target volumes to prescribe for IS.
9/ Two Cochrane reviews with thousands of patients undergoing upper abdominal (UAS) and cardiac surgery show that IS is no more effective than standard physical therapy, deep breathing exercises, or even no intervention in preventing PPCs.
pubmed.ncbi.nlm.nih.gov/24510642/
pubmed.ncbi.nlm.nih.gov/24510642/
10/ Even randomized control trials of high-risk cohorts undergoing bariatric or thoracic surgery show no benefit to IS in preventing PPCs. Yet despite a lack of evidence it's estimated that the US healthcare system spends >$1 Billion annually on IS.
pubmed.ncbi.nlm.nih.gov/30175643/
pubmed.ncbi.nlm.nih.gov/30175643/
11/ In 2011 The American Association for Respiratory Care published guidelines recommending against using IS alone to prevent PPCs in UAS and cardiac surgery patients . They recommend IS only as a part of a multimodal approach to care.
pubmed.ncbi.nlm.nih.gov/22008401/
pubmed.ncbi.nlm.nih.gov/22008401/
12/ The best data for IS comes from I-COUGH which included IS in rigorous standardized postoperative treatment plan.
The downside? The study didn't look at which of the various individual components made a difference so it's unclear how much IS helped.
pubmed.ncbi.nlm.nih.gov/23740240/
The downside? The study didn't look at which of the various individual components made a difference so it's unclear how much IS helped.
pubmed.ncbi.nlm.nih.gov/23740240/
13/ So if IS doesn't work to prevent PPCs, what should we do instead? Until there's better data, it's not clear we need to do anything instead. Early mobilization and telling patients to take deep breaths on a schedule without a device appear to work just as well as IS.
14/ Are there times where we should use IS?
For patients at particularly high-risk for PPCs, the benefits of IS for the individual may outweigh the risks since there's both little benefit and little risk.
For patients at particularly high-risk for PPCs, the benefits of IS for the individual may outweigh the risks since there's both little benefit and little risk.
15/ IS may also be beneficial as a preoperative intervention along with inspiratory muscle training in helping high-risk patients prepare for scheduled surgery. IS has a role in helping with recovery from rib fractures and in vaso-occlusive crisis in Sickle Cell Disease
16/ So what are the key takeaways?
🫁Atelectasis is common after surgery
🫁There is little evidence supporting the routine use of incentive spirometry in reducing postoperative pulmonary complications
🫁Consider early mobilization or deep breathing exercises as alternatives
🫁Atelectasis is common after surgery
🫁There is little evidence supporting the routine use of incentive spirometry in reducing postoperative pulmonary complications
🫁Consider early mobilization or deep breathing exercises as alternatives
For more details read our newest publication in @JHospMedicine Things We Do for No Reason: Routine use of incentive spirometry to reduce postoperative pulmonary complications!
…mpublications.onlinelibrary.wiley.com/doi/epdf/10.10…
@SatyaPatelMD @kelleychuang @jaimebetancourt
#TWDFNR
…mpublications.onlinelibrary.wiley.com/doi/epdf/10.10…
@SatyaPatelMD @kelleychuang @jaimebetancourt
#TWDFNR
• • •
Missing some Tweet in this thread? You can try to
force a refresh