"Indoor Air Management of Airborne Pathogens: Lessons, Practices, and Innovations" eventbrite.com/e/indoor-air-m…
Workshop by @theNASEM focusing on the current state of knowledge ➡️ practical lessons learned. Session 1 starting now.
Live-tweets below
#EHMI #NASEM #EnviroHealthMatters

Workshop by @theNASEM focusing on the current state of knowledge ➡️ practical lessons learned. Session 1 starting now.
Live-tweets below
#EHMI #NASEM #EnviroHealthMatters


2/ @Don_Milton summarizes evidence that saliva PCR much better at catching COVID positive cases than PCR from nasal swabs. 



3/ @Don_Milton: It's the *combination* of masks, ventilation, filtration that can dramatically reduce spread 

4/ @Don_Milton: But it's super-spreading (a few people drive the spread to huge number of others) that has been driving the pandemic.
Masks are important, but needs engineering controls to make biggest impact.

Masks are important, but needs engineering controls to make biggest impact.


5/ @Don_Milton: "Extensive evidence for airborne transmission." This is no longer the question
Testing and vaccination are insufficient to prevent transmission.
Layers including environmental interventions are key.

Testing and vaccination are insufficient to prevent transmission.
Layers including environmental interventions are key.


6/ @ShellyMBoulder gives "The Miller Report" on lessons learned about engineering controls to reduce exposure and viral aerosol spread of COVID. 
7/ @ShellyMBoulder summarizing work showing that direction of airflow through apartment building matters. Engaging experienced engineers, even adding fans in selected areas, can make a huge difference. 



8/ @ShellyMBoulder: Plenty of evidence that ventilation and filtration reduces airborne load of SARS-CoV-2 virus 

9/ @ShellyMBoulder summarizes another cool study that HEPA filtration can have a positive effect by reducing aerosol concentration in a local area within a room, not only the total aerosol load of the room. 

10/ @ShellyMBoulder summarizes recent studies she led to evaluate amount of infectious SARS-CoV-2 aerosol & exposure risk using various engineering strategies in various building types: offices, schools, more
e.g. sciencedirect.com/science/articl…
e.g. sciencedirect.com/science/articl…

11/ @ShellyMBoulder summary:
* Ventilation and air cleaning reduce viral aerosol loads indoors
* In-room germicidal UV is the only air cleaning strategy to universally reduce risk to acceptable levels in all buildings in all scenarios (and so is masking!)
* Ventilation and air cleaning reduce viral aerosol loads indoors
* In-room germicidal UV is the only air cleaning strategy to universally reduce risk to acceptable levels in all buildings in all scenarios (and so is masking!)

12/ #EHMI How do we move toward a better balance between energy & cost?
@ShellyMBoulder: Upper-room UV is much more cost-effective than re-doing whole HVAC system. In general, need E-efficient ventilation/filtration. DIY #CorsiRosenthalBox cleaners are also very cost-effective.
@ShellyMBoulder: Upper-room UV is much more cost-effective than re-doing whole HVAC system. In general, need E-efficient ventilation/filtration. DIY #CorsiRosenthalBox cleaners are also very cost-effective.

13/ #EHMI What about UV?
@ShellyMBoulder: 254 nm in upper-room; Decades of evidence it can work very well to reduce room exposure. An important part of a total response.
@Don_Milton: Doing work with "far UV" now. Relatively eye-safe; doesn't need to be isolated in upper rom.
@ShellyMBoulder: 254 nm in upper-room; Decades of evidence it can work very well to reduce room exposure. An important part of a total response.
@Don_Milton: Doing work with "far UV" now. Relatively eye-safe; doesn't need to be isolated in upper rom.
14/ @Lakdawala_Lab: Fascinating that it has been shown that fewer than 10 particles are necessary (in cases) to initiate infection. This knowledge plays into how we think about ventilation, filtration, UV mitigation strategy. Close-range exposure also important to keep in mind.
15/ #EHMI What type of practical steps are most promising at the building-level to reduce respiratory virus transmission?
Malin Alsved: Ventilation. Designing buildings to keep talking volume in mind so people don't have to shout, b/c talking volume scales with aerosol emission.
Malin Alsved: Ventilation. Designing buildings to keep talking volume in mind so people don't have to shout, b/c talking volume scales with aerosol emission.
16/ #EHMI Practical steps continued ...
Bill Lindsley: Portable air cleaners.
@Don_Milton: Pay attention to both long and short-range transmission. All the controls in combination is the solution.
Bill Lindsley: Portable air cleaners.
@Don_Milton: Pay attention to both long and short-range transmission. All the controls in combination is the solution.
17/ #EHMI Practical steps continued ...
@ShellyMBoulder: Love to emphasize embracing more use of UV in all types of public spaces, especially plus energy-efficient ventilation/filtration
Yuguo Li: Avoid superspreading events by improving the worst buildings with very poor ACH
@ShellyMBoulder: Love to emphasize embracing more use of UV in all types of public spaces, especially plus energy-efficient ventilation/filtration
Yuguo Li: Avoid superspreading events by improving the worst buildings with very poor ACH
18/ #EHMI Practical steps continued ...
@Lakdawala_Lab: Not all viruses went away b/c modes of transmission are slightly different. Need multiple strategies to mitigate all modes.
@Lakdawala_Lab: Not all viruses went away b/c modes of transmission are slightly different. Need multiple strategies to mitigate all modes.
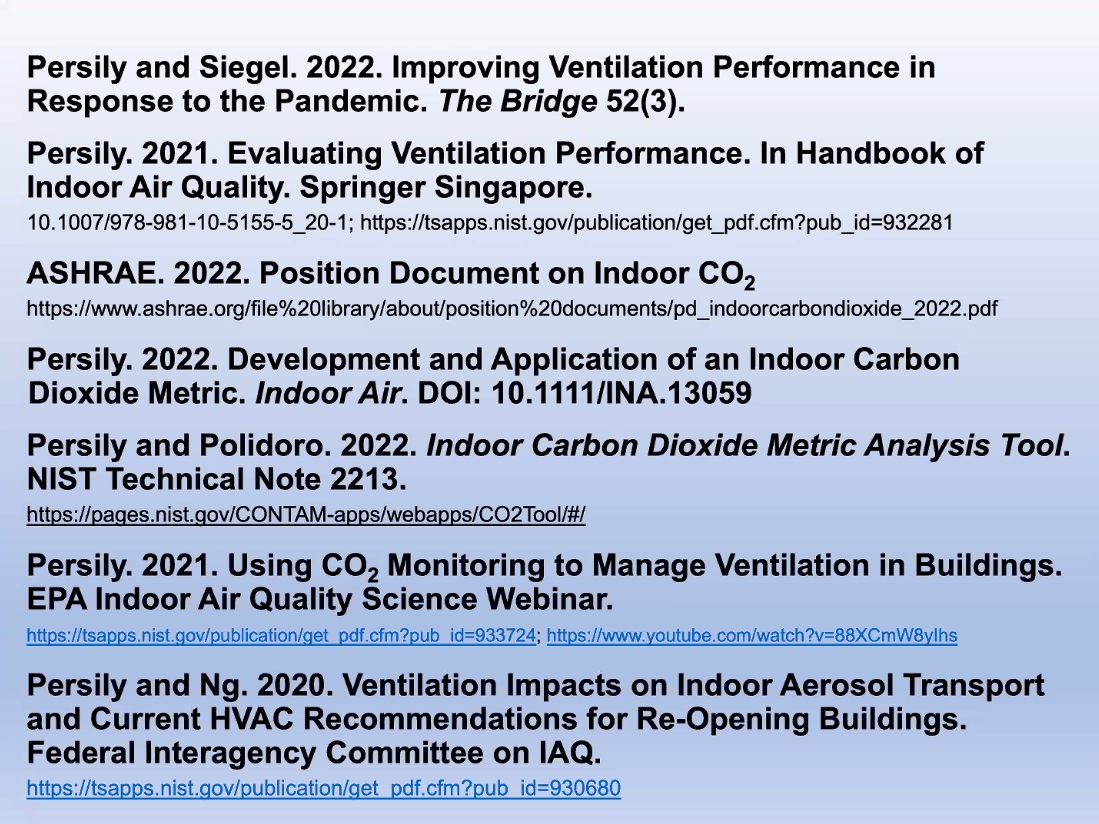
20/ #EHMI: Andy Persily
To better improve indoor air quality & reduce airborne aerosol spread, improving ventilation is key. But no one-size fits all answers. Need to assess for targeted improvements.
To better improve indoor air quality & reduce airborne aerosol spread, improving ventilation is key. But no one-size fits all answers. Need to assess for targeted improvements.

21/ #EHMI Andy Persily
* Measuring CO2 can be very useful, but have to be careful to understand the details.
* Don't just measure CO2 in isolation, you need to understand context in room.
* One CO2 threshold for all rooms not sufficient. It's about per-person emission rate.

* Measuring CO2 can be very useful, but have to be careful to understand the details.
* Don't just measure CO2 in isolation, you need to understand context in room.
* One CO2 threshold for all rooms not sufficient. It's about per-person emission rate.


22/ #EHMI Andy Persily
*Managing & improving ventilation isn't rocket science, but you need to know some things to do it well. Engage engineers.
* Measuring CO2 can be useful, but a quick glance at a number isn't sufficient to really understand the space.

*Managing & improving ventilation isn't rocket science, but you need to know some things to do it well. Engage engineers.
* Measuring CO2 can be useful, but a quick glance at a number isn't sufficient to really understand the space.

23/ @stephensbrent gives an overview of the types of air cleaning technologies. Each work by different strategies & provide different benefits. Additive & subtractive technologies. 

24/ @stephensbrent: Evaluate technology for air cleaning by using data!
CADR (Clean Air Delivery Rate) is key, but make sure units & meaning interpreting correctly.

CADR (Clean Air Delivery Rate) is key, but make sure units & meaning interpreting correctly.
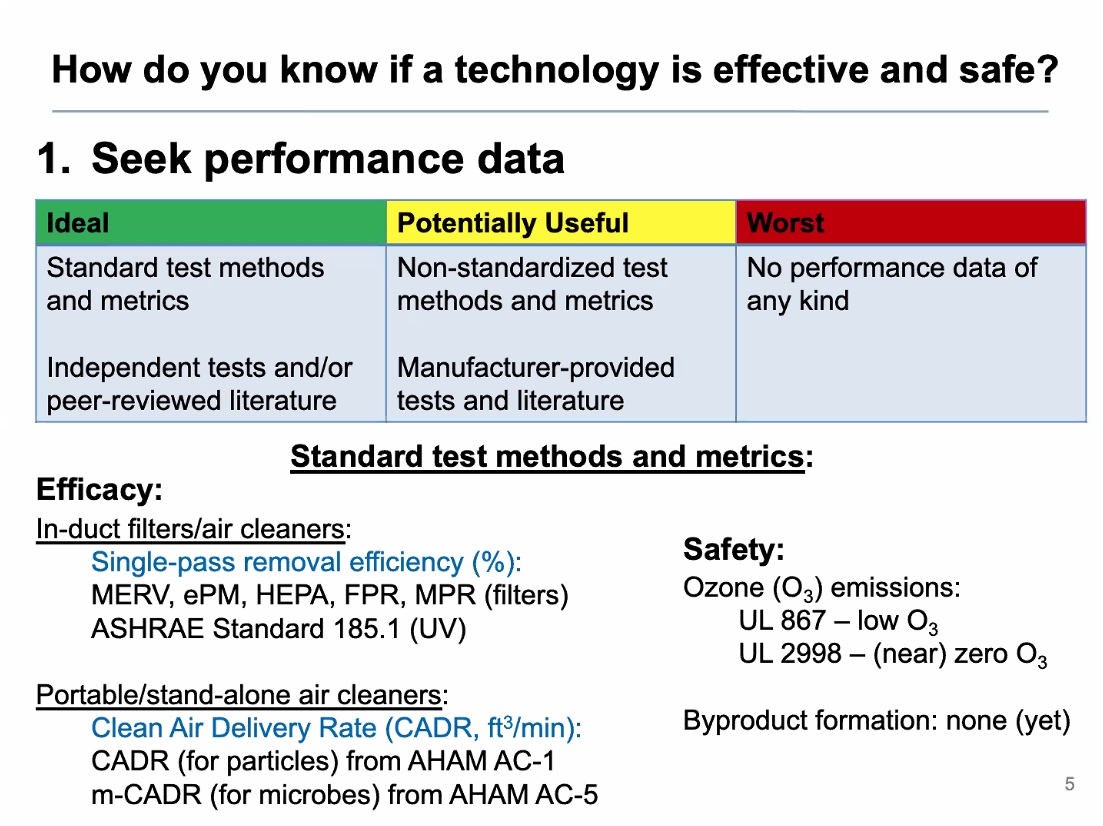

25/ @stephensbrent Highlights a tool available via @etgall et al. to look at air cleaner efficiency: pdx.edu/healthy-buildi… 

26/ @EwanEadie Introduces the idea of UV, between 200 - 280 nm, for viral inactivation. #UVGI #UpperRoomUV 





27/ @EwanEadie: "A wealth of evidence" that UV works (echos the repeated refrain today by @ShellyMBoulder @Don_Milton) 



28/ @EwanEadie further discusses the safety of UV, #UVGI. Long-standing data showing human safety. Also still additional work being done. 



29/ #EHMI Where should we put CO2 monitors in a room?
@Wymelenberg: Somewhere accessible. Ideally put CO2 monitor near return air vent to get average of room.
Andy Persily: Definitely not close to exhalation sources (misleading signals; not room background) or supply air vent.
@Wymelenberg: Somewhere accessible. Ideally put CO2 monitor near return air vent to get average of room.
Andy Persily: Definitely not close to exhalation sources (misleading signals; not room background) or supply air vent.

30/ #EHMI How can we convince medical professionals to accept aerosol transmission of infectious disease?
Difficult question for this panel, but @Wymelenberg: Anecdotes working recently in hospitals - *Collaboration* between aerosol scientists/engin & med. professionals is key!
Difficult question for this panel, but @Wymelenberg: Anecdotes working recently in hospitals - *Collaboration* between aerosol scientists/engin & med. professionals is key!
31/ #EHMI Are UV sources dangerous from photochemistry they can initiate?
@WBahnfleth: Not major problem. See Ch. 5 of the report on NASEM indoor air chemistry: nap.nationalacademies.org/catalog/26228/…
Katherine Ratliff: Also research into chemistry at surfaces.
Persily: Keep maintenance in mind
@WBahnfleth: Not major problem. See Ch. 5 of the report on NASEM indoor air chemistry: nap.nationalacademies.org/catalog/26228/…
Katherine Ratliff: Also research into chemistry at surfaces.
Persily: Keep maintenance in mind
32/ Other good comments in #NASEM #EHMI Session 2 by @WBahnfleth, @marwa_zaatari, but too fast for me to keep up.
Half-way through the sessions; scheduled break. Join at:
"Indoor Air Management of Airborne Pathogens: Lessons, Practices, and Innovations" eventbrite.com/e/indoor-air-m…
Half-way through the sessions; scheduled break. Join at:
"Indoor Air Management of Airborne Pathogens: Lessons, Practices, and Innovations" eventbrite.com/e/indoor-air-m…
33/ CY Wu in Session 2 of #EHMI webinar on indoor management of airborne pathogens.
"Most people make a wise decision when relevant information is provided." Emphasizes that data
& collaboration between relevant engineers/scientists is necessary to inform decisions & policy.

"Most people make a wise decision when relevant information is provided." Emphasizes that data
& collaboration between relevant engineers/scientists is necessary to inform decisions & policy.


34/ Summary by CY Wu of a study led by @vfmcneill showing ventilation & CO2 data from a variety of schools & universities:
* Collection of data can be important to help motivate action.
* Ventilation quality can vary widely (at schools).

https://twitter.com/HuffmanLabDU/status/1487086854327336968
* Collection of data can be important to help motivate action.
* Ventilation quality can vary widely (at schools).


35/ #EHMI CY Wu also showed a summary of one part of my lab's contribute to the study by @vfmcneill et al. last year: sciencedirect.com/science/articl…
Providing CO2 data in university music classrooms helped reveal ventilation schedule problems, easy solutions:
Providing CO2 data in university music classrooms helped reveal ventilation schedule problems, easy solutions:
https://twitter.com/HuffmanLabDU/status/1335999099166810115?s=20&t=Ckf2VLNQsPOTrjJVhBX59g

36/ Conclusions by CY Wu:
* Simple clear messaging important to public health
* Most people make a wise decision when relevant info provided
* Don't assume consistency of language
* Policy & technology innovation are complementary; collaborate + build trust
(Thx @Iamgoingtosleep)
* Simple clear messaging important to public health
* Most people make a wise decision when relevant info provided
* Don't assume consistency of language
* Policy & technology innovation are complementary; collaborate + build trust
(Thx @Iamgoingtosleep)

37/ Prof. Dr. Sandra Crouse Quinn provides imp. context about the relationship b/n the individual community and the science or policies provided.
Communication is key. Engineering is only part of the solution. Successful efforts to put #CRBox air cleaners in various communities.
Communication is key. Engineering is only part of the solution. Successful efforts to put #CRBox air cleaners in various communities.
38/ Reverend Anthony Evans of @NBCIBlackChurch talks about moving from the science-phase of the pandemic to community action
Looking at air quality, policies, measuring air. Will share data. As clergy, no one told us to do this. This will be for the betterment of all society! 👏

Looking at air quality, policies, measuring air. Will share data. As clergy, no one told us to do this. This will be for the betterment of all society! 👏


39/ #EHMI webinar
Peg Seminario (AFC-IO): We have to keep equity closely in mind with our understanding and response. Black and Latinx communities have been far more deeply impacted by COVID and continue to be. Response & help needs to be considered accordingly.
#UrgencyofEquity
Peg Seminario (AFC-IO): We have to keep equity closely in mind with our understanding and response. Black and Latinx communities have been far more deeply impacted by COVID and continue to be. Response & help needs to be considered accordingly.
#UrgencyofEquity

40/ David Rowson (EPA) talks about the wide-reaching co-benefits of improving indoor air quality, well beyond "just" reducing infectious disease.
Makes me think of this table summarizing data making the same point:
Makes me think of this table summarizing data making the same point:
https://twitter.com/HuffmanLabDU/status/1386892817402720257?s=20&t=7gm2vC_aJrbd3EvR97jaYg
41/ #EHMI
* CY Wu: Clear communication b/n parties
* Rev. Anthony Evans: Importance of trust b/n community & leaders. MLK Jr: No tension b/n religion & science.
* David Rowson: Trust! Fumbled this w/ COVID. Public awareness of indoor air quality only just beginning; at a new age.
* CY Wu: Clear communication b/n parties
* Rev. Anthony Evans: Importance of trust b/n community & leaders. MLK Jr: No tension b/n religion & science.
* David Rowson: Trust! Fumbled this w/ COVID. Public awareness of indoor air quality only just beginning; at a new age.
43/ #EHMI panel wrap-up fireside chat
Tomas Aragon (@CAPublicHealth): Summarizes the California "SMARTER" plan - covid19.ca.gov/smarter/
Shots
Masks
Awareness
Readiness
Testing
Education
Rx
Tomas Aragon (@CAPublicHealth): Summarizes the California "SMARTER" plan - covid19.ca.gov/smarter/
Shots
Masks
Awareness
Readiness
Testing
Education
Rx
44/ #EHMI fireside chat
@WBahnfleth: Important to recognize that this broader discussion cannot be separately about 'indoor air quality' and 'reducing pathogen transmission.' They have to be the same conversation.
@WBahnfleth: Important to recognize that this broader discussion cannot be separately about 'indoor air quality' and 'reducing pathogen transmission.' They have to be the same conversation.
45/ #EHMI fireside chat
@Jon_Samet, @WBahnfleth: We had similar bioaerosol convos 20 & 30 years ago, but not nearly enough change happened. One difference now (in contrast to anthrax, 9/11 motivations), COVID brought the immediacy of public health need into everyone's life & home
@Jon_Samet, @WBahnfleth: We had similar bioaerosol convos 20 & 30 years ago, but not nearly enough change happened. One difference now (in contrast to anthrax, 9/11 motivations), COVID brought the immediacy of public health need into everyone's life & home
46/ #EHMI fireside chat
Peg Seminario: Emphasized several times how important it is to closely engage w/ stake-holders on the ground. Often public health agencies are good but may not have sufficient awareness of issues w/in all groups (nursing homes, correctional facilities …)
Peg Seminario: Emphasized several times how important it is to closely engage w/ stake-holders on the ground. Often public health agencies are good but may not have sufficient awareness of issues w/in all groups (nursing homes, correctional facilities …)
47/ #EHMI fireside chat
John Howard (NIOSH): Looking back at what we've learned, it took a lot of time to get past the focus on large droplets falling down quickly. Wanted data specifically w/ SARS-CoV-2 first.
Now we know that "aerosol transmission is a real thing." (‼️)
John Howard (NIOSH): Looking back at what we've learned, it took a lot of time to get past the focus on large droplets falling down quickly. Wanted data specifically w/ SARS-CoV-2 first.
Now we know that "aerosol transmission is a real thing." (‼️)
48/ #EHMI fireside chat
@WBahnfleth: Regarding implementation of mitigations against airborne spread, we had a lot of suggestive evidence invoking the precautionary principle. Then it took a lot of time to convince. In the meantime we could have done *a lot* more good for people.
@WBahnfleth: Regarding implementation of mitigations against airborne spread, we had a lot of suggestive evidence invoking the precautionary principle. Then it took a lot of time to convince. In the meantime we could have done *a lot* more good for people.
49/ #EHMI fireside chat
Tomas Aragon (CA DPH):
How do we help people make decisions in a situation of uncertainty? There's always complexity and uncertainty.
Balance between when we should give recommendations vs requirements. Getting that balance right is a real challenge.
Tomas Aragon (CA DPH):
How do we help people make decisions in a situation of uncertainty? There's always complexity and uncertainty.
Balance between when we should give recommendations vs requirements. Getting that balance right is a real challenge.
50/ #EHMI fireside chat
Shawn Ryan (EPA): Balance between research questions and what is really needed to push out into the community.
Shawn Ryan (EPA): Balance between research questions and what is really needed to push out into the community.
51/ David Rowson:
Need to deal w/ psychology of risk & individual impression. Indoor air quality issue is received very differently without reaction.
For long-term change, we need to continue educating that #IAQ is one of the biggest factors in health quality for all of us.
Need to deal w/ psychology of risk & individual impression. Indoor air quality issue is received very differently without reaction.
For long-term change, we need to continue educating that #IAQ is one of the biggest factors in health quality for all of us.
52/ Peg Seminario (AFL-CIO): We can't make sufficient change individually. System needs to change.
Much of the government guidance on COVID is *way* out of date. Bring it up to date! E.g., it would help if CDC would come out and make very clear statements that #COVIDisAirborne.
Much of the government guidance on COVID is *way* out of date. Bring it up to date! E.g., it would help if CDC would come out and make very clear statements that #COVIDisAirborne.
54/ Rapid, wrap-up summary of @theNASEM #EHMI workshop on "Indoor Air Management of Airborne Pathogens: Lessons, Practices, and Innovations"; By organizers @linseymarr & @Jon_Samet
First, there is "overwhelming evidence" that COVID is transmitted through aerosols: LM
First, there is "overwhelming evidence" that COVID is transmitted through aerosols: LM
55/ @linseymarr summary of #EHMI sessions 1,2:
1⃣ Ventilation, filtration, UV, masks all important components to mitigate infectious disease spread
2⃣ Engineering controls are efficient and important components to reduce infectious airborne disease transmission
1⃣ Ventilation, filtration, UV, masks all important components to mitigate infectious disease spread
2⃣ Engineering controls are efficient and important components to reduce infectious airborne disease transmission
56/ @linseymarr summary of #EHMI sessions 1,2:
3⃣ Higher ventilation rate is better; >6 ACH ideal, but varies based on number of people, activity type, and interpersonal differences in physiology, emission rates, etc. (superspreaders)
3⃣ Higher ventilation rate is better; >6 ACH ideal, but varies based on number of people, activity type, and interpersonal differences in physiology, emission rates, etc. (superspreaders)
57/ @linseymarr summary of #EHMI sessions 1,2:
4⃣ Start with the basics: make sure ventilation, #IAQ system is designed well and operating as designed
5⃣ Once basics are covered, then optimize the system. Evaluate with data, engaging experts; CO2 useful, but not silver bullet.
4⃣ Start with the basics: make sure ventilation, #IAQ system is designed well and operating as designed
5⃣ Once basics are covered, then optimize the system. Evaluate with data, engaging experts; CO2 useful, but not silver bullet.
58/ @linseymarr summary of #EHMI sessions 1,2:
6⃣ UV, including far-UV can be an important component of the overall IAQ and airborne respiratory disease strategy; long-standing evidence; more research will continue to establish details and further fill-in gaps in understanding
6⃣ UV, including far-UV can be an important component of the overall IAQ and airborne respiratory disease strategy; long-standing evidence; more research will continue to establish details and further fill-in gaps in understanding
59/ @linseymarr summary of #EHMI sessions 1,2:
7⃣ "We have a lot of tools to improve IAQ and reduce airborne disease transmission. It's time to open up the toolbox, make sure they work, and use them to make healthier indoor environments." 👏
7⃣ "We have a lot of tools to improve IAQ and reduce airborne disease transmission. It's time to open up the toolbox, make sure they work, and use them to make healthier indoor environments." 👏
60/ @Jon_Samet summary of #EHMI sessions 3, 4:
* Overview of why we are or are not using the strategies that work
* Several models will be useful as case studies, e.g.:
- work by Rev. Anthony Evans and @NBCIBlackChurch
- work by @CAPublicHealth
(see tweets above)
* Overview of why we are or are not using the strategies that work
* Several models will be useful as case studies, e.g.:
- work by Rev. Anthony Evans and @NBCIBlackChurch
- work by @CAPublicHealth
(see tweets above)
61/ @Jon_Samet summary of #EHMI sessions 3, 4:
* Need to continue advancing the scientific foundation of respiratory infectious disease transmission
* Need leadership at the national level!
* Upcoming planning from White House & other agencies will help determine what comes next
* Need to continue advancing the scientific foundation of respiratory infectious disease transmission
* Need leadership at the national level!
* Upcoming planning from White House & other agencies will help determine what comes next
62/ @Jon_Samet summary of #EHMI sessions 3, 4:
* Surveillance & evaluation are still areas that need work to be able to quickly, routinely assess risks and active aerosol spread of specific pathogens within an indoor air space.
* Surveillance & evaluation are still areas that need work to be able to quickly, routinely assess risks and active aerosol spread of specific pathogens within an indoor air space.
63/ @Jon_Samet summary of #EHMI sessions 3, 4:
* Many building types; need to know how well they're each working, have surveillance tools & deployment that works well for each
* Overview of process ⬇️, but diagram needs loops to put efficacious approaches into action
@linseymarr
* Many building types; need to know how well they're each working, have surveillance tools & deployment that works well for each
* Overview of process ⬇️, but diagram needs loops to put efficacious approaches into action
@linseymarr

64/ @Jon_Samet summary of #EHMI sessions 3, 4:
* There are different time domains in terms of what we know works. For things that can be operational & effective now - "Get on with it!"
(Linking to earlier in the discussion; comments by @WBahnfleth ⬇️)
* There are different time domains in terms of what we know works. For things that can be operational & effective now - "Get on with it!"
(Linking to earlier in the discussion; comments by @WBahnfleth ⬇️)
https://twitter.com/HuffmanLabDU/status/1560343155748192258?s=20&t=GPTbJtT1TtkOarQ4P-0hmQ
65/ That closes my live-tweets of #EHMI workshop on "Indoor Air Management of Airborne Pathogens: Lessons, Practices, & Innovations" - nationalacademies.org/our-work/indoo…
Great work @linseymarr & @Jon_Samet!
Stay tuned for workshops 2 & 3 in the series. Coming: schools & public transport
Great work @linseymarr & @Jon_Samet!
Stay tuned for workshops 2 & 3 in the series. Coming: schools & public transport

66/ Page with video of the full workshop and links to slide decks from each presentation now available via NASEM.
(Thx to @citlanx for the alert)
nationalacademies.org/event/07-21-20…
(Thx to @citlanx for the alert)
nationalacademies.org/event/07-21-20…
• • •
Missing some Tweet in this thread? You can try to
force a refresh


















