Greatly enjoyed launching our @MGH_PCCM @HarvardPulm didactic critical care echo curriculum with LV Assessment - Beyond the Eyeball!
Assessing LV function isn't as simple as it sounds.
Take home messages for POCUS learners below ⤵️:
#POCUS #Echofirst #Medtwitter #PCCMTwitter


Assessing LV function isn't as simple as it sounds.
Take home messages for POCUS learners below ⤵️:
#POCUS #Echofirst #Medtwitter #PCCMTwitter
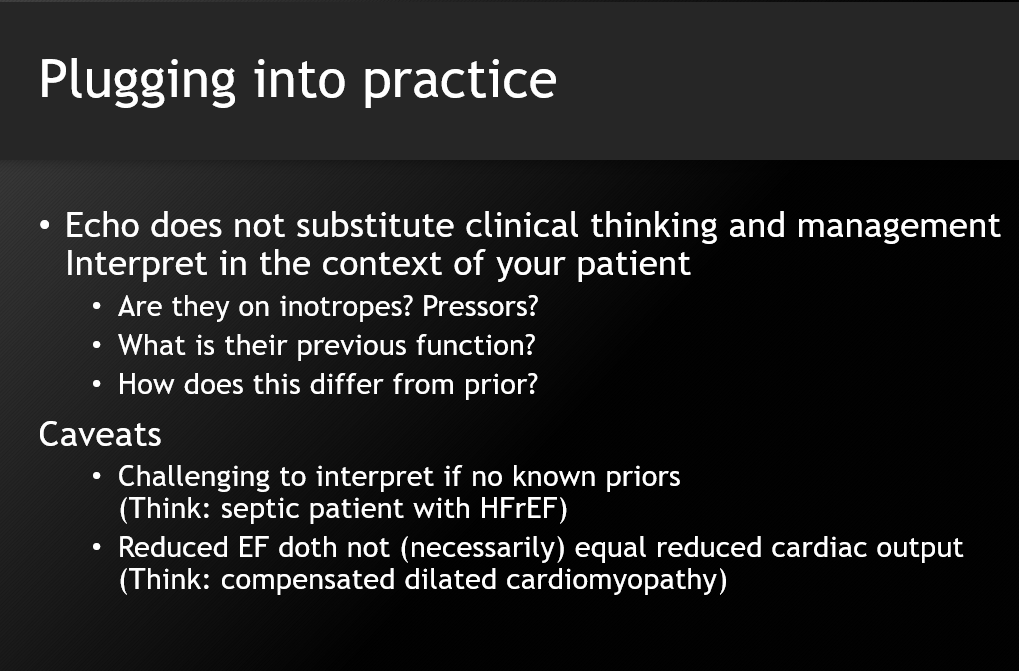
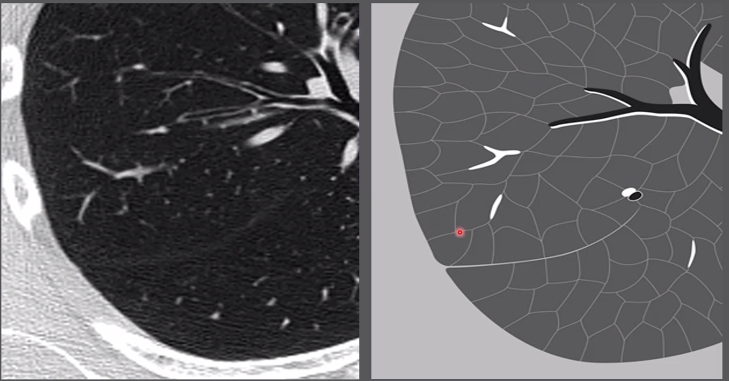
👀The oft-invoked 'eyeball' method is a deceptive oversimplification. You can't suddenly accurately assess LV function just because you're told to!
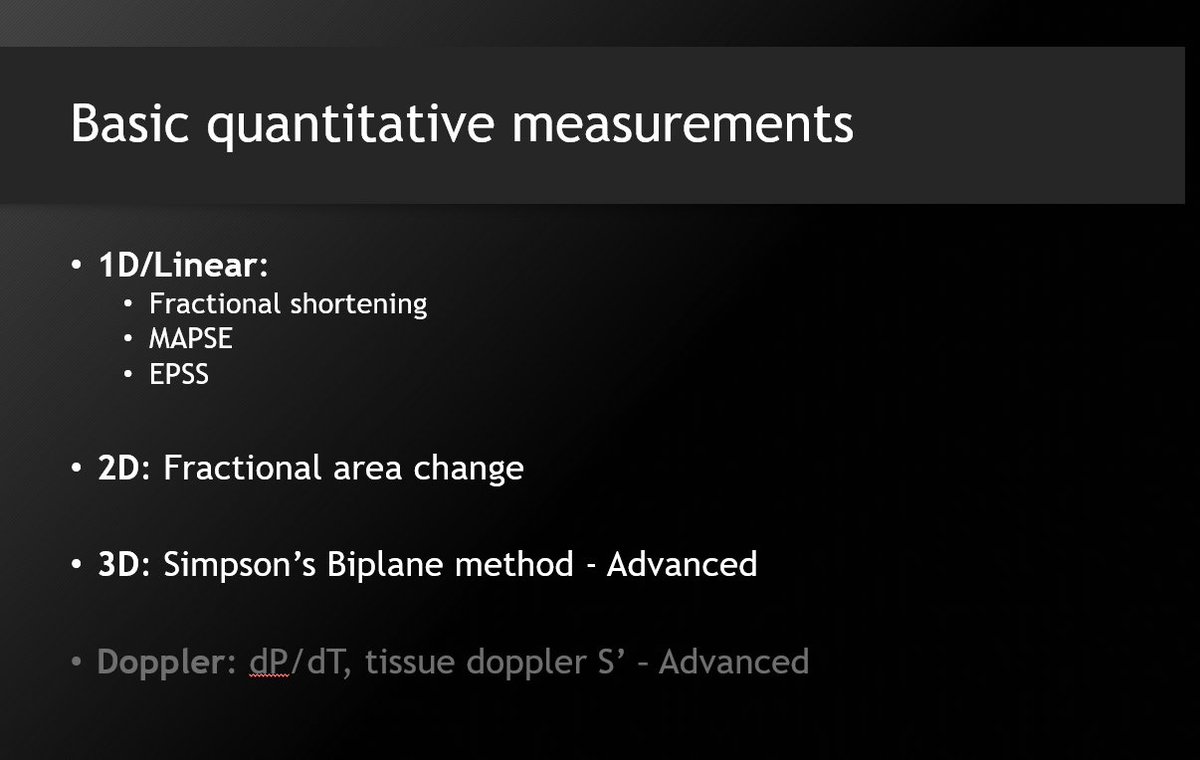
You need to train your eye to look at other quantifiable measures of LF function - even if you won't actually measure them. 🧐
You need to train your eye to look at other quantifiable measures of LF function - even if you won't actually measure them. 🧐
Sure - make your best guesstimate of EF. But also look at:
1⃣myocardial thickening
2⃣myocardial excursion
3⃣annular excursion/MAPSE
4⃣fractional shortening +/- fractional area change
5⃣EPSS
You don't have to actually measure these, but you can't 'see' them if you don't know them!
1⃣myocardial thickening
2⃣myocardial excursion
3⃣annular excursion/MAPSE
4⃣fractional shortening +/- fractional area change
5⃣EPSS
You don't have to actually measure these, but you can't 'see' them if you don't know them!
💡My suggestion: Go ahead and actually learn how to measure these, and do each one 10+ times. You will train/refine your eye to accurately eyeball the next one. The more you do, the more subtle differences you'll be able to pick up. It's surprisingly easy to learn!
This does take 'basic' echo a bit into what I would call 'intermediate', but the returns are powerful. Welcome others' input: @khaycock2 @msiuba @MaxHockstein @katiewiskar @siddharth_dugar @The_echo_lady @echonepean @nickmmark @ThinkingCC @cameron_baston @pocusmeded @EchoSoliman
Can follow if interested in basic-intermediate POCUS content. Intend to be sharing highlights/takeaways from all our critical care lectures/conferences this year!
Critical care echo* lectures. Important qualifier.
• • •
Missing some Tweet in this thread? You can try to
force a refresh