Diuretic management in decompensated heart failure has been stagnant for years but recently we have some new tools to help us out.
Let's review the Rise of the Proximal Tubule Inhibitors in preparation for the #nephjc discussion on ADVOR tonight.
#MedTwitter @MedTweetorials
Let's review the Rise of the Proximal Tubule Inhibitors in preparation for the #nephjc discussion on ADVOR tonight.
#MedTwitter @MedTweetorials
First, it's important to recognize how crucial adequate decongestion is.
👇study: pubmed.ncbi.nlm.nih.gov/29544928/ which assessed pts in the PROTECT trial showed lack of decongestion was a predictor of mortality and HF re-hospitalization
Another one by Metra: pubmed.ncbi.nlm.nih.gov/22167320/
👇study: pubmed.ncbi.nlm.nih.gov/29544928/ which assessed pts in the PROTECT trial showed lack of decongestion was a predictor of mortality and HF re-hospitalization
Another one by Metra: pubmed.ncbi.nlm.nih.gov/22167320/

Only a minority of patients in the DOSE trial, which used high dose diuretics were free from congestion at 72 hours
nejm.org/doi/full/10.10…
nejm.org/doi/full/10.10…

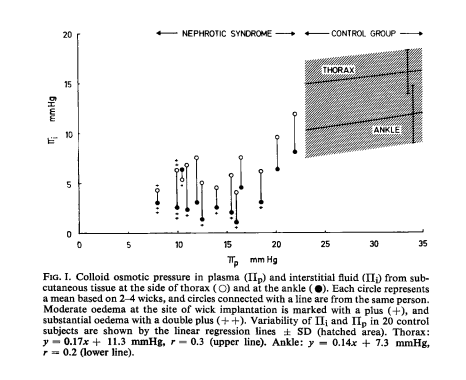
To gauge success we need a target. Traditional parameters like weights and Is/Os may not be appropriate.
There was no correlation seen among these parameters and outcomes when looking at participants in DOSE, ESCAPE and Penn trials
👉pubmed.ncbi.nlm.nih.gov/25595470/
There was no correlation seen among these parameters and outcomes when looking at participants in DOSE, ESCAPE and Penn trials
👉pubmed.ncbi.nlm.nih.gov/25595470/

What has been shown is that net negative sodium balance matters, A LOT. An assessment of participants in ROSE with 24h urine collections, net negative Na balance was associated with improved 6 mo survival. Net fluid balance and weight loss were not.
👉pubmed.ncbi.nlm.nih.gov/31047017/
👉pubmed.ncbi.nlm.nih.gov/31047017/

This prospective study of 110 pts showed if spot UNa didn't ⬆️ post furosemide = sig higher mortality as well as higher NGAL and KIM-1. Shows the importance of following spot UNa levels in response to diuretics - as well as "door to decongestion time"
onlinelibrary.wiley.com/doi/full/10.10…
onlinelibrary.wiley.com/doi/full/10.10…

A number of studies have now looked at spot UNa values to assess natriuresis and this has been part of our practice @UWNephrology for the past 2 years.
A clinical trial looking at the utility of UNa to guide decongestion is currently recruiting.
clinicaltrials.gov/ct2/show/NCT05…
A clinical trial looking at the utility of UNa to guide decongestion is currently recruiting.
clinicaltrials.gov/ct2/show/NCT05…

Ok on to proximal tubule inhibitors. We know that diuretic resistance is common and a major proposed mech is distal nephron hypertrophy with ⬆️ NCC channels. Adding thiazide diuretics is common and makes physiologic sense but data is lacking outside of CARRESS. 



💡majority of Na reab. in the prox tubule (up to 85%). Makes sense to🛑this, but efficacy limited by distal sites of reab.
Diamox = 1st non-mercurial diuretic but quickly forgotten after losing the war to loops (expected)
Nice thread by @ChristosArgyrop
Diamox = 1st non-mercurial diuretic but quickly forgotten after losing the war to loops (expected)
Nice thread by @ChristosArgyrop
https://twitter.com/ChristosArgyrop/status/1563551593873584128?s=20&t=t_o5m3-xLTAn-_NoCgVN0w
Enter ADVOR, which is the largest diuretic RCT to date
🎆n=519 pts with ADHF + volume overload
🎆500mg IV diamox daily v placebo
🎆All pts received loop diuretics
🎆primary endpoint: successful decongestion @72 hours
Diamox=more natriuresis and 12% more pts dry after 72 hours

🎆n=519 pts with ADHF + volume overload
🎆500mg IV diamox daily v placebo
🎆All pts received loop diuretics
🎆primary endpoint: successful decongestion @72 hours
Diamox=more natriuresis and 12% more pts dry after 72 hours


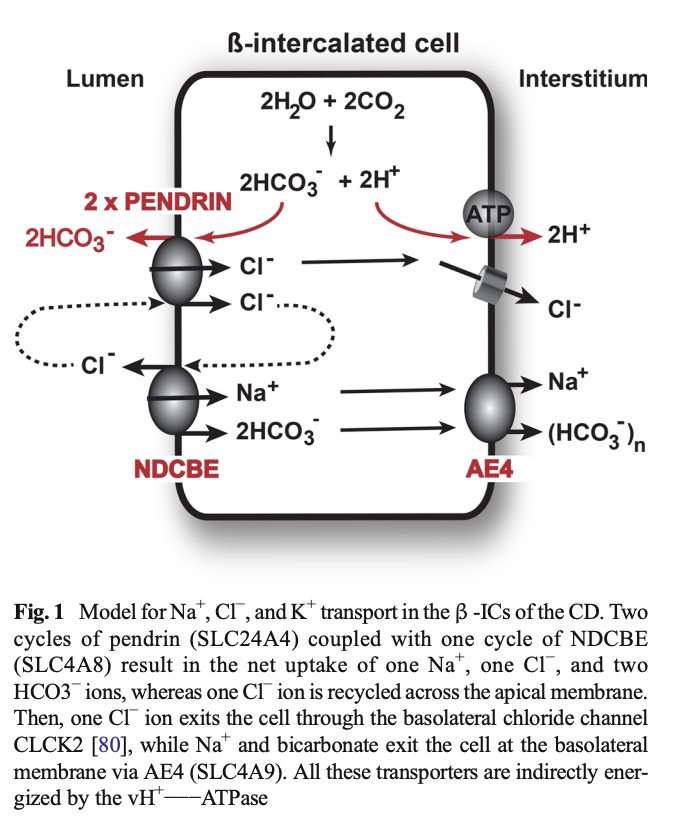
@ChristosArgyrop suggests some of the success may be due to diamox inhibiting pendrin (intercalated cells upregulated in HF)
Based on this paper: pubmed.ncbi.nlm.nih.gov/24260196/
Tho this paper suggests the mech may be thiazide sensitive: pubmed.ncbi.nlm.nih.gov/20389022/


Based on this paper: pubmed.ncbi.nlm.nih.gov/24260196/
Tho this paper suggests the mech may be thiazide sensitive: pubmed.ncbi.nlm.nih.gov/20389022/
https://twitter.com/captainchloride/status/1455642739933003776?s=20&t=LTuVQMxQiICKs5IgDkGr2A


What about the OTHER prox tubule inhibitors #flozins?
Esp. relevant in light of EMPULSE showing benefit in starting empa in-hospital pubmed.ncbi.nlm.nih.gov/35228754/
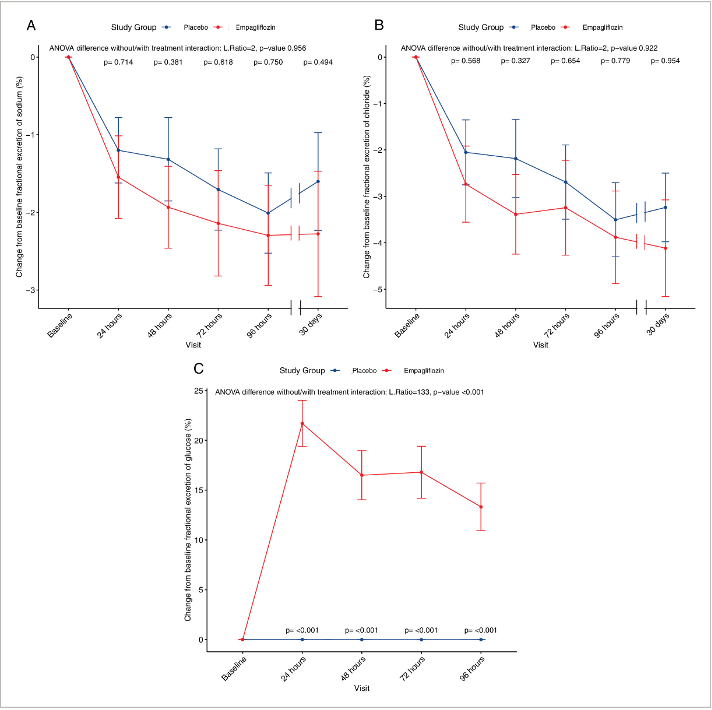
👇study showed ⬆️natriuresis and ⬇️blood volume without NH activation when flozins added to loops
pubmed.ncbi.nlm.nih.gov/32410463/

Esp. relevant in light of EMPULSE showing benefit in starting empa in-hospital pubmed.ncbi.nlm.nih.gov/35228754/
👇study showed ⬆️natriuresis and ⬇️blood volume without NH activation when flozins added to loops
pubmed.ncbi.nlm.nih.gov/32410463/


Earlier this year EMPAG-HF was published
🎆single center placebo controlled trial
🎆randomized pts with ADHF to empa 25 or placebo w/in 12 hours
🎆All pts got loops
🎆Endpoint: UOP over 5d
Result: 25% ⬆️UOP and ⬆️diuretic efficiency
pubmed.ncbi.nlm.nih.gov/35766022/
🎆single center placebo controlled trial
🎆randomized pts with ADHF to empa 25 or placebo w/in 12 hours
🎆All pts got loops
🎆Endpoint: UOP over 5d
Result: 25% ⬆️UOP and ⬆️diuretic efficiency
pubmed.ncbi.nlm.nih.gov/35766022/

This may make physiologic sense since it appears Angiotensin II upregulates SGLT2 channels, which is very relevant in patients with heart failure
pubmed.ncbi.nlm.nih.gov/31375080/
pubmed.ncbi.nlm.nih.gov/31375080/

Problem: Unclear if ⬆️UOP from natriuresis or osmotic diuresis. As opposed to the☝️ 2019 study, this showed empa = glycosuria w/out natriuresis
pubmed.ncbi.nlm.nih.gov/33251643/
Likely d/t distal Na reabsorption, whereas not poss. w/ glu. I wonder if this would be better with loops+thiaz

pubmed.ncbi.nlm.nih.gov/33251643/
Likely d/t distal Na reabsorption, whereas not poss. w/ glu. I wonder if this would be better with loops+thiaz

Conclusions:
🔥We are in the era of proximal tubule inhibitors
🔥I want to see diamox and flozins tested in diuretic resistance
🔥Would be nice to compare diamox v flozins
🔥I'm also interested in diamox + flozins given distinct mech
In the meantime tune in to #nephjc tonight!
🔥We are in the era of proximal tubule inhibitors
🔥I want to see diamox and flozins tested in diuretic resistance
🔥Would be nice to compare diamox v flozins
🔥I'm also interested in diamox + flozins given distinct mech
In the meantime tune in to #nephjc tonight!
• • •
Missing some Tweet in this thread? You can try to
force a refresh