Tweetorial on #vasodilators for low-output #heartfailure
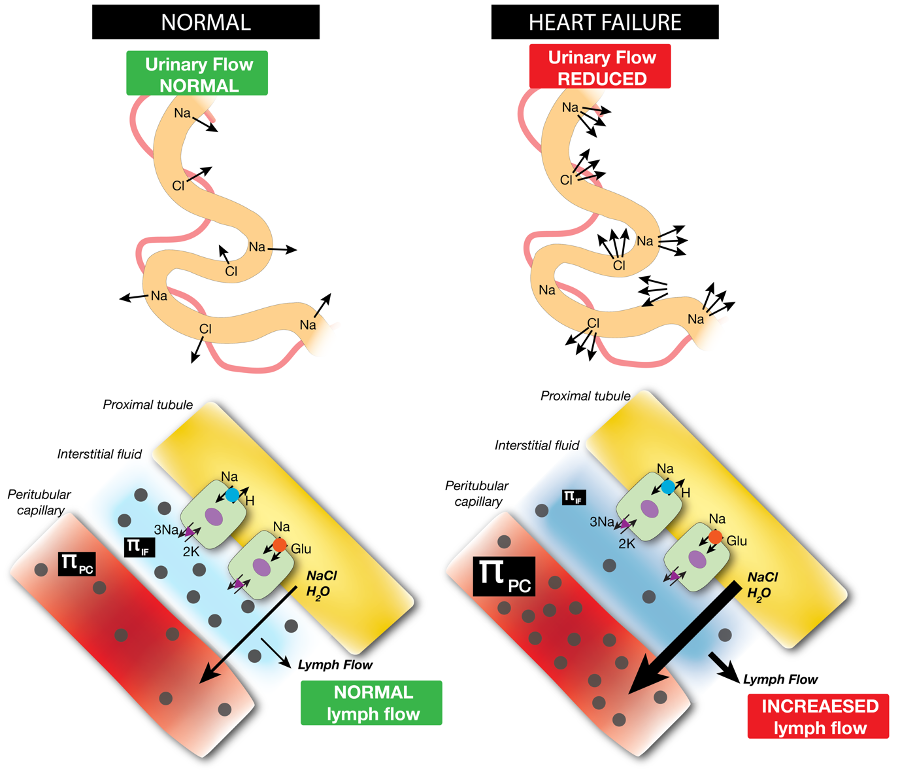
to improve hemodynamics which help to decongest better and allow introduction/uptitration of neurohumorel blockers.
(as addendum to
to improve hemodynamics which help to decongest better and allow introduction/uptitration of neurohumorel blockers.
(as addendum to
https://twitter.com/FH_Verbrugge/status/1578947788855205888) (1/10)
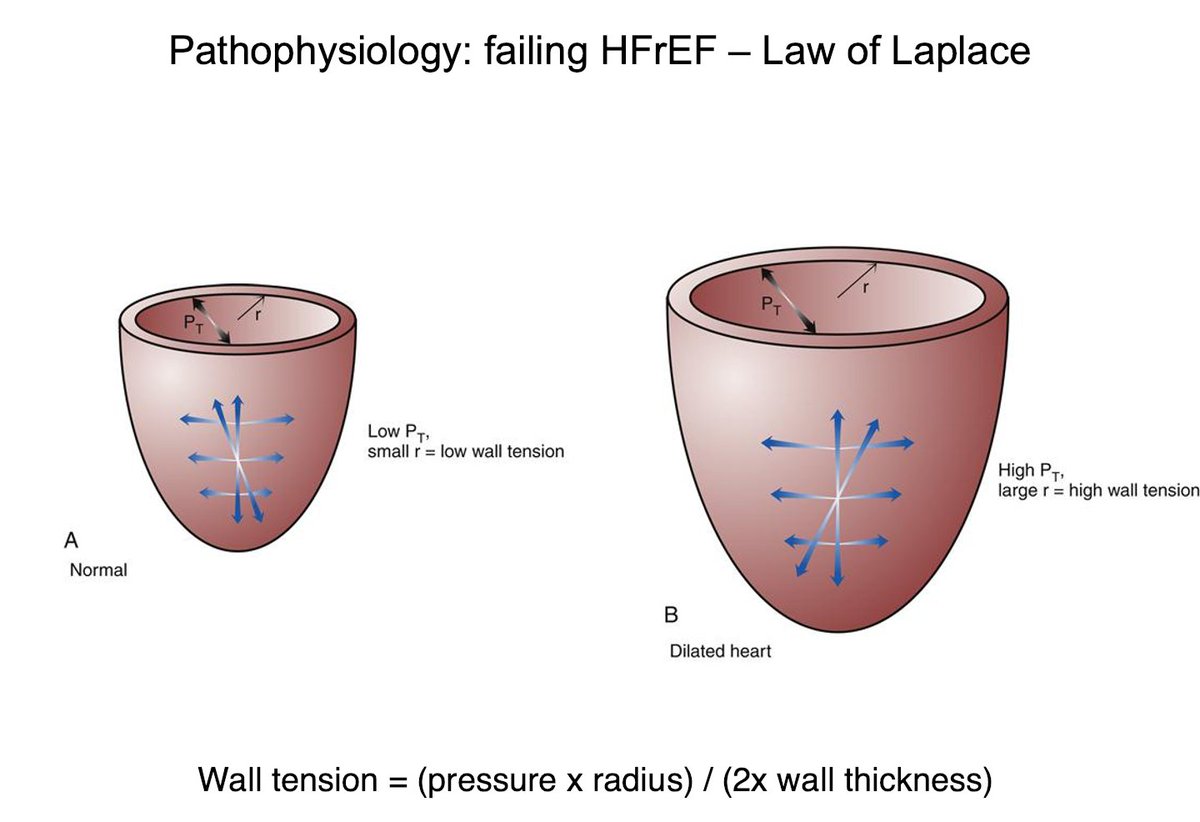
High afterload in failing HFrEF (not HFpEF) is also strongly determined by ⬆️ wall tension (not SVR) as ⬆️ R and ⬇️ wall thickness. SVR is an oversimplification of afterload. (5/10) 
Vasodilator ⬆️ cardiac output in failing HFrEF through reduction of afterload often with =/⬆️ blood pressure
(6/10)
(6/10)

Nr 1 vasoactive agent to use in failing HFrEF (cold+wet) = nitroprusside with dose adjustment based upon MAP. Inotropes in this situation = medical error as they induce often "crash and burn scenario" (ie addition of vasopressors - MCS which should NOT have occurred).....(7/10) 

See nitroprusside for low-output critical AS (surely afterload is not determined by SVR as AS is fixed resistance, but it's also wall tension) (8/10)
25 patient study in @NEJM pubmed.ncbi.nlm.nih.gov/12724481/
25 patient study in @NEJM pubmed.ncbi.nlm.nih.gov/12724481/

See nitroprusside for low-output decompensated HFrEF pubmed.ncbi.nlm.nih.gov/18617068/ (9/10) 

see also @NMHheartdoc (10/10)
@AlexMebazaa @PieterMartensMD @WilsonTangMD @rcstarling @HanCardiomd @HSkouri @luisbeckdasilva @FinnGustafsson
@AlexMebazaa @PieterMartensMD @WilsonTangMD @rcstarling @HanCardiomd @HSkouri @luisbeckdasilva @FinnGustafsson

• • •
Missing some Tweet in this thread? You can try to
force a refresh