Sometimes pancreatitis involves the duodenum, let´s talk about paraduodenal/groove pancreatitis
Don't miss this #GItwitter thread based on my talk for @harvardmed @HMSPostgradCE #HarvardMINT2022 course
Thanks, @CharuParanjape @krishnanendo for one of my best experiences ever!
Don't miss this #GItwitter thread based on my talk for @harvardmed @HMSPostgradCE #HarvardMINT2022 course
Thanks, @CharuParanjape @krishnanendo for one of my best experiences ever!

Pancreas inflammation involving the duodenum has many names: Cystic dystrophy on aberrant pancreas of the duodenal wall, Groove pancreatitis... Adsay and Zamboni proposed paraduodenal pancreatitis as a term that involves these 2 organs 

There are 2 important concepts:
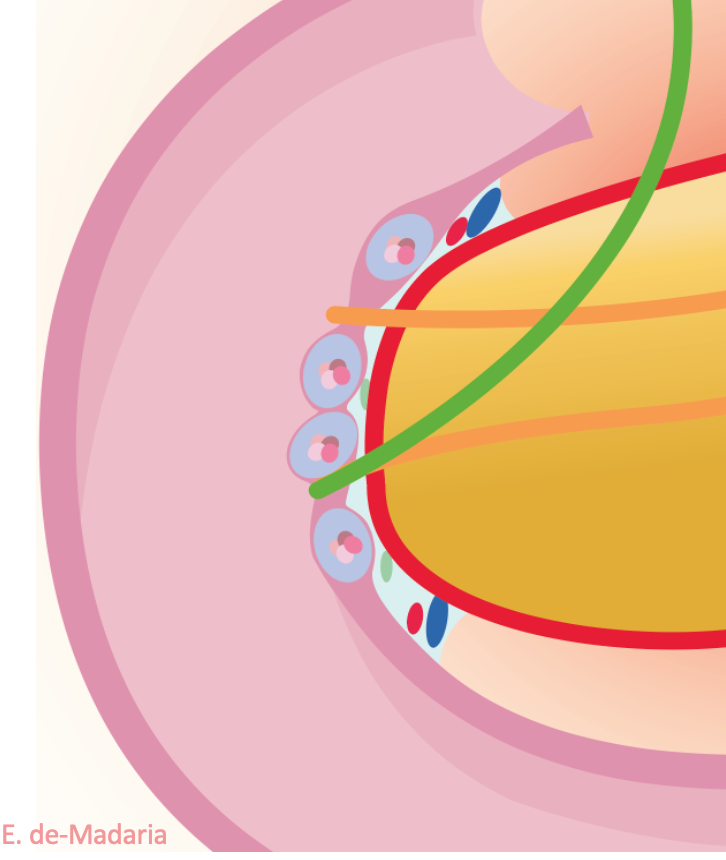
1) The pancreatic-duodenal groove is the space between the duodenum and the pancreas: vessels, lymph nodes, Wirsung, Santorini, CBD & some acini are there. Those acini can suffer from pancreatitis: that`s groove pancreatitis
1) The pancreatic-duodenal groove is the space between the duodenum and the pancreas: vessels, lymph nodes, Wirsung, Santorini, CBD & some acini are there. Those acini can suffer from pancreatitis: that`s groove pancreatitis

2) Some people have ectopic pancreatic tissue within the duodenal wall, those acini may have inflammation 

Prof. Becker looked for surgical specimens with groove inflammation among 600 chronic pancreatitis patients who underwent Whipple procedure, 20% had groove involvement: 2% pure, 7% groove+pancreatic head involvement, 11% groove + classic chronic pancreatitis 

Most patients with paraduodenal pancreatitis have alcoholic + smoke etiology for their pancreatic inflammation (and that´s my experience) 

According to 1 single center study 0.18% of all pathology samples have digestive wall heterotopic pancreatic tissue, in 25% cases in duodenum/proximal jejunum
sciencedirect.com/science/articl…
sciencedirect.com/science/articl…

When that ectopic acini within the duodenal wall become inflamed, we had what has been called cystic dystrophy on ectopic pancreas of the duodenal wall: cysts within the duodenal wall, thickened duodenal wall, this can be seen very well by EUS @japariciot2 @Belenmm271 


Paraduodenal pancreatitis symptoms & signs: gastric outlet obstruction, jaundice, pain, weight loss and diarrhea (due to pancreatic exocrine insufficiency) 

In CT scan we can identify different patterns of paraduodenal pancreatitis:
- Pure cystic: this is the "cystic dystrophy of the duodenal wall"
- Solid-cystic: both
- Pure solid: that´s "groove pancreatitis"

- Pure cystic: this is the "cystic dystrophy of the duodenal wall"
- Solid-cystic: both
- Pure solid: that´s "groove pancreatitis"


The pancreatic gland may be involved or not, most patients will have pancreatic gland features of chronic pancreatitis
BE CAREFUL MY FRIEND, there is something evil called pancreatic groove adenocarcinoma, a pancreatic cancer involving the pancreatic duodenal groove
sciencedirect.com/science/articl…
These signs may help to differentiate malignant from benign stuff
sciencedirect.com/science/articl…
These signs may help to differentiate malignant from benign stuff

This is the endoscopic view of paraduodenal pancreatitis, from my colleagues from @HospitalLaFe Pedro López Muñoz and @vicen_pons thieme-connect.com/products/ejour… 

And you can see the USE findings in this video from Dario Ligresti and colleagues
thieme-connect.com/products/ejour…
thieme-connect.com/products/ejour…

Few studies have been published focused on paraduodenal pancreatitis management, have a look at this systematic review from Kager et al
journals.lww.com/jcge/Abstract/…
👇👇👇
journals.lww.com/jcge/Abstract/…
👇👇👇

Patients with PERSISTING pain without big cysts and those with PERSISTING gastric outlet obstruction may benefit from surgery when conservative treatment is not working 

Some conclusions, I hope you liked the review and my drawings, all crafted with great excitement as my first @harvardmed @HMSPostgradCE collaboration! 

Now it is time for you to retweet the first tweet of the thread 😁
@p_lopezmunoz crack gracias!
@GVAsalualicante @isabial_iis @GVAsanitat @UniversidadMH @dmedicina_umh @MedicinaUmh @MclinicaUMH @RectorUMH
@surgeon_young @jutifler @DharJahnvi @Jayanta_sam @e_santino @med020064 @NataliaCorzo12 @EurPancClub @TeamSurgery247 @renzopc77 @sanjay_HPB @lelecapurso @manuknayar @TarekNammour @CHPBAsurg @rcverdonk @Jesus_Ruiz_Man @GIPapachristou @CristinaP_25 @my_ueg @AISP_Pancreas
• • •
Missing some Tweet in this thread? You can try to
force a refresh