NEXT :: COPD - Oriole Roca.
Evidence : NIV is great for acute COPD. The classic from Laurent Brochard pubmed.ncbi.nlm.nih.gov/7651472/
Evidence : NIV is great for acute COPD. The classic from Laurent Brochard pubmed.ncbi.nlm.nih.gov/7651472/
but if beyond 24 hours. alternative is High flow nasal cannulae.
#LIVES2022
#ventilation
#NIV #COPD @ESICM
#LIVES2022
#ventilation
#NIV #COPD @ESICM
@ESICM NIV failure - intubat the patient, COPD patient intubated, Vol Control, 7ml/kg PBW, I:E = 1:4 , RR 20. Then patient is "hypotensive". why?
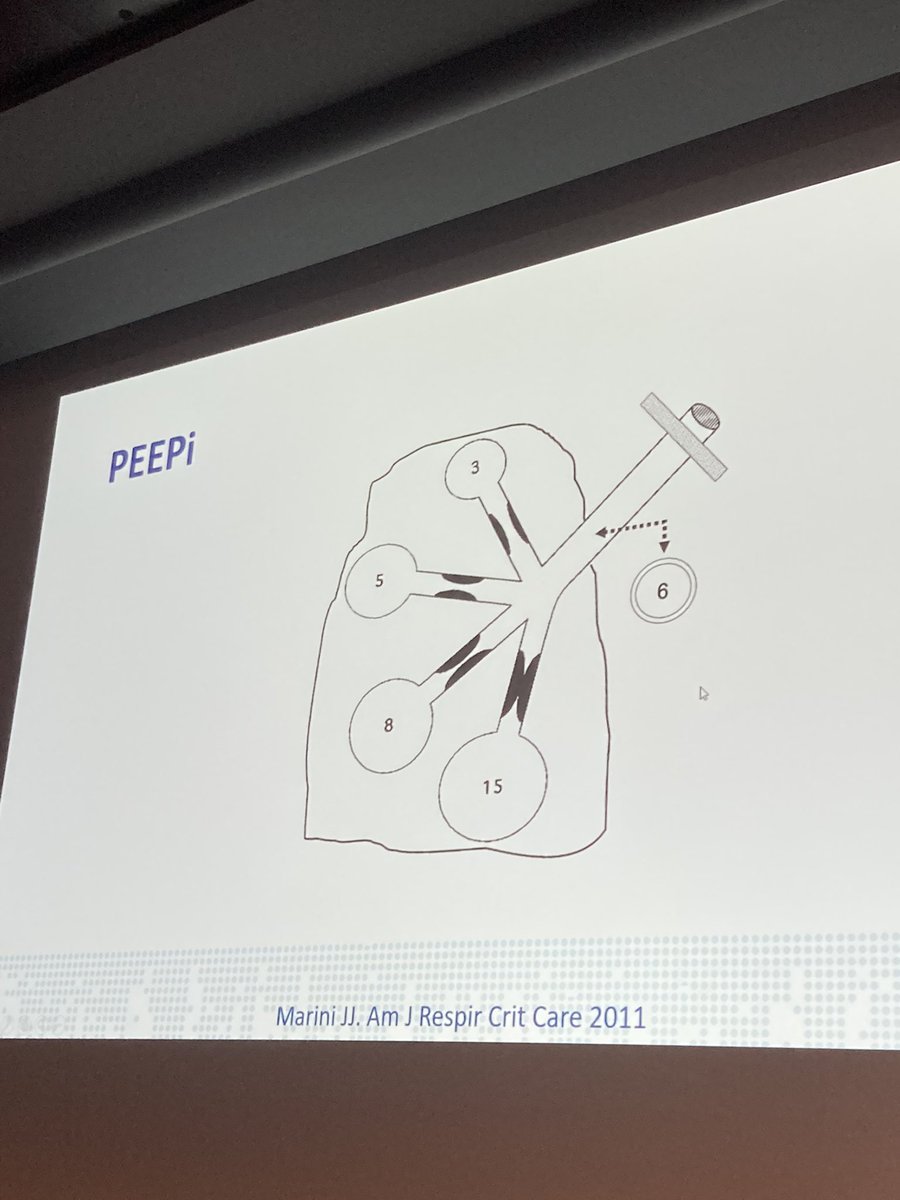
@ESICM "Dynamic Hyperinflation". Consequences : Barotrauma, Haemodynamic instability, Asynchrony. How do we quantify dynamic hyperinflation? a). volume end-inspiration b). Pplat c).intrinsic PEEP d).None of them.
@ESICM What is "volume end-inspiration"? Disconnect from breathing circuit and measure the inspiratory volume trapped. Vei <20ml/kg -> low res kof barotrauma / Haemodynamic instability. original paper in 1987
Thus, we undertake "intrinsic PEEP'. iPEEP may be an under-estimate.
Thus, we undertake "intrinsic PEEP'. iPEEP may be an under-estimate.
further expansion by Lisanne. pubmed.ncbi.nlm.nih.gov/34862945/
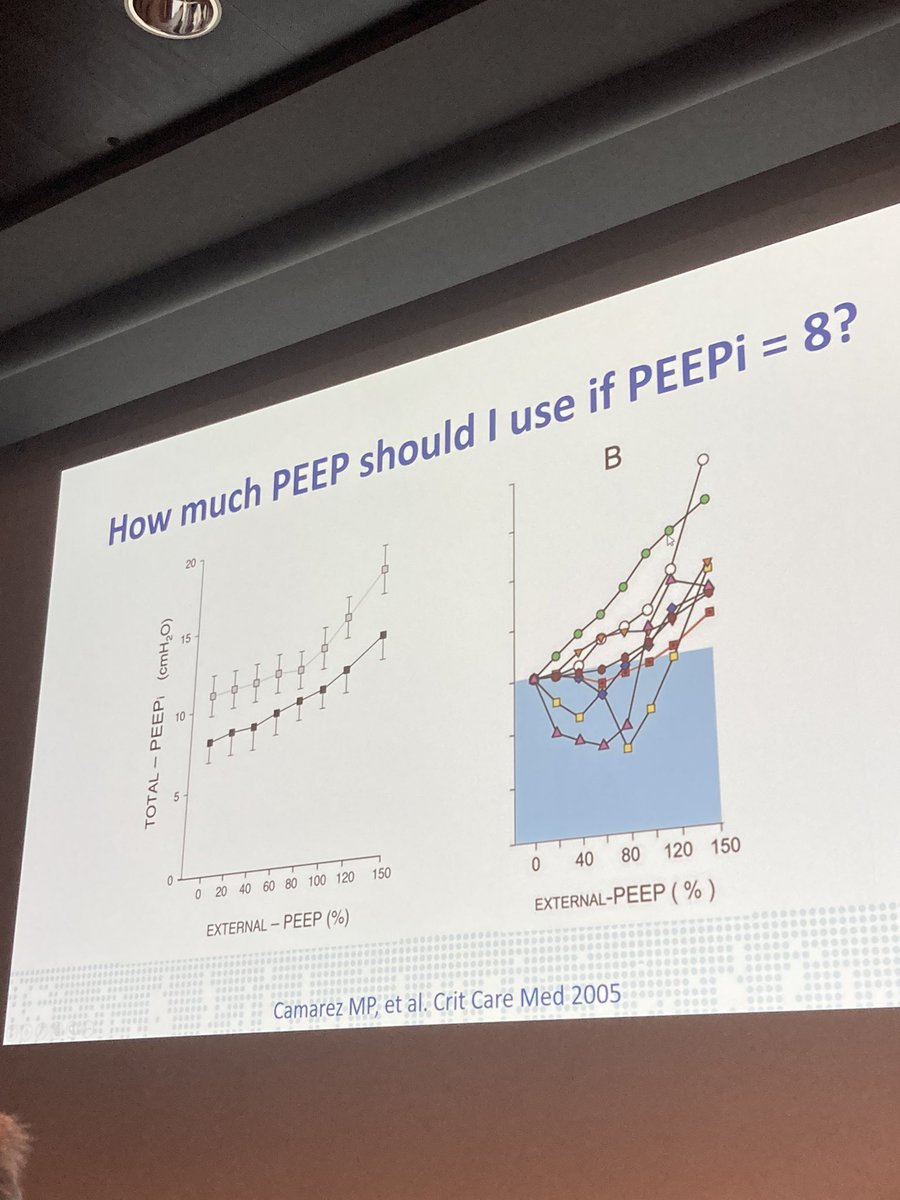
How much PEEP should be used if iPEEP = 8 and patient is relaxed?
a). ZEEP b). PEEP 5 c). PEEP 8. d). Not use PEEPi to set external PEEP
a). ZEEP b). PEEP 5 c). PEEP 8. d). Not use PEEPi to set external PEEP
pubmed.ncbi.nlm.nih.gov/16003057/
Above link paper: Why is this? This is because applying different levels of PEEP stents the airway.
as a result, try any of the 3 options BUT be prepared to change depending on how your pt phenotype.
Above link paper: Why is this? This is because applying different levels of PEEP stents the airway.
as a result, try any of the 3 options BUT be prepared to change depending on how your pt phenotype.
These patients also have higher asynchronies due to the extra lung volume.
pubmed.ncbi.nlm.nih.gov/12821570/
Again P oes can be used to detect intrinsic PEEP.
pubmed.ncbi.nlm.nih.gov/12821570/
Again P oes can be used to detect intrinsic PEEP.
Finally, 1st line treatment COPDe = NIV (?HfNO potentially). Quantify and Rx dynamic hyperinflation. Don't care about ABG. PEEP setting during controlled vs. assisted MV.
Summary paper : pubmed.ncbi.nlm.nih.gov/33169215/
Summary paper : pubmed.ncbi.nlm.nih.gov/33169215/
Audience ?1: ECCO2R with or without NIV is a possibility? Luigi Camporota : yes possible sometimes to prevent intubation or to help facilitate extubation and minimise muscle loss, etc. Q2: in terms of SpO2 target, best to go with patient's own spo2 - not higher or lower.
Q3. What about "cor pulmonale"? The theme is emerging which is that you need to combine the respiratory and cardiovascular. intubation these patients with cor pulmonale could have significant consequences. The holistic care. #WeAreICU #TogetherICU #IntensiveCare #CriticalCare
Q4. Awake proning on NIV for COPD patients? No evidence - individually tried from the expert panel - not great anecdotal experiences.
• • •
Missing some Tweet in this thread? You can try to
force a refresh